Cross-cultural adaptation and psychometric properties of the Chinese version of the Intermittent Self-Catheterization Questionnaire (ISC-Q)
- Published
- Accepted
- Received
- Academic Editor
- Yoshinori Marunaka
- Subject Areas
- Nursing, Urology
- Keywords
- Neurogenic lower urinary tract dysfunction, Intermittent self-catheterization, Quality of life, Cross-cultural adaptation, Psychometric properties
- Copyright
- © 2024 Hu et al.
- Licence
- This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits using, remixing, and building upon the work non-commercially, as long as it is properly attributed. For attribution, the original author(s), title, publication source (PeerJ) and either DOI or URL of the article must be cited.
- Cite this article
- 2024. Cross-cultural adaptation and psychometric properties of the Chinese version of the Intermittent Self-Catheterization Questionnaire (ISC-Q) PeerJ 12:e18226 https://doi.org/10.7717/peerj.18226
Abstract
Background
The intermittent self-catheterization questionnaire (ISC-Q) is a valid and reliable tool to assess the quality of life (QOL) in patients with neurogenic lower urinary tract dysfunction (NLUTD) who engage in ISC. The aim of this research is to culturally adapt the ISC-Q and evaluate its psychometric properties within the Chinese patient population.
Methods
The cross-sectional research was meticulously conducted in two pivotal stages: initially, the focus was on cross-cultural adaptation, followed by an extensive phase of psychometric testing. This comprehensive analysis involved 405 Chinese patients with NLUTD who use ISC. Various analyses, including evaluations of the floor and ceiling effects, item analysis, content validity, exploratory and confirmatory factor analysis (EFA and CFA), assessments of convergent, discriminant, and criterion validity. Additionally, Cronbach’s alpha was utilized to determine internal consistency, and test-retest reliability was measured using the intraclass correlation coefficient (ICC).
Results
No floor and ceiling effects were observed. The content validity index was 0.967. The EFA identified four factors, accounting for 64.953% of the total variance, and this four-factor structure was confirmed by the CFA. The fit indices in CFA were favorable, with χ2/df = 1.999, root mean square error of approximation = 0.070, comparative fit index = 0.916, Tucker–Lewis index = 0.900, goodness-of-fit index = 0.863, and incremental fit index = 0.917. The average variance extracted for the four factors ranged from 0.466 to 0.565, with composite reliability values ranging from 0.776 to 0.859. The ISC-Q showed a positive correlation with the intermittent self-catheterization acceptance questionnaire (r = 0.557, P < 0.001). The ICC overall Cronbach’s alpha coefficient for the questionnaire was 0.821, and the for test-retest reliability was 0.951 (95% CI [0.900–0.976] P < 0.001).
Conclusion
The validity and reliability of the Chinese version of the ISC-Q have been verified, making it suitable for measuring the QOL in NLUTD patients who practice ISC.
Introduction
Neurogenic lower urinary tract dysfunction (NLUTD) is prevalent among patients with neurological disorders, particularly in those with spinal cord injuries (70–84%), stroke (up to 53%), Parkinson’s disease (38–71%), and multiple sclerosis (32–96%) (Zhao et al., 2022). Managing NLUTD is complex; intermittent self-catheterization (ISC) is the recommended practice in guidelines due to its significant advantages in reducing infection risks, preserving patient dignity, and enhancing treatment effectiveness compared to other bladder management methods (Prieto et al., 2021; Ginsberg et al., 2021). Despite these guidelines, adherence to ISC remains suboptimal, with utilization rates around 50% in Western countries and compliance rates near 20% (Gharbi et al., 2022). The situation is even more concerning in China, where ISC usage plummets to approximately 26% (Zhou et al., 2021).
For NLUTD patients, evaluating the quality of life (QOL) is crucial for their adoption and adherence to ISC (Newman et al., 2020; Wang et al., 2021a; Gharbi et al., 2022). Implementing ISC directly impacts the patients’ daily life and mental health (Seth, Haslam & Panicker, 2014; Goldstine et al., 2019). The inconvenience of carrying and using catheters can limit their activities and social interactions (Beauchemin et al., 2018). Concerns about safety and hygiene may lead to anxiety and fear, with prolonged psychological stress potentially resulting in social isolation and depression (Yılmaz et al., 2014; Palmer, 2021). Therefore, accurately assessing and improving QOL is vital to enhancing the acceptance and adherence to ISC, necessitating the reliance on scientific and effective assessment tools.
Generally, QOL is assessed using patient-reported outcome measures (PROMs) (Łaszewska et al., 2022), which is one of the key indicators of health outcomes related to ISC (Wang et al., 2021a). PROMs are indispensable tools for assessing patients’ health status, treatment response, and changes in quality of life (Shunmuga Sundaram et al., 2022). For patients with NLUTD who require frequent ISC, the application of PROMs is particularly crucial (Wang et al., 2021a). PROMs provide NLUTD patients with a direct channel to express their feelings and needs, enabling healthcare professionals to comprehensively understand the patients’ experience and outcomes with ISC treatment. This understanding facilitates precise adjustments to treatment strategies, ultimately leading to a significant improvement in the patients’ quality of life (Wang et al., 2021a).
To accurately assess the QOL related to ISC, in 2012, Pinder et al. (2012) developed a QOL tool specifically for ISC, covering ease of use, convenience, discreetness, and psychological Well-being aspects. This tool has been proven to be reliable and effective. It aims to measure patients’ QOL and identify barriers to ISC, serving as a cornerstone for interventions to improve ISC usage and adherence rates, thereby enhancing patient treatment outcomes. Consequently, this tool has been translated into multiple languages, including Turkish (Yeşil et al., 2020), Korean (Kang et al., 2019), Italian (Scivoletto et al., 2017), Dutch (Hervé et al., 2019), and Japanese (Yoshida et al., 2017), and has been widely used in numerous studies.
Despite the global application of the ISC-Q assessment tool, there has been a lack of comprehensive validation and adaptability assessment among the Chinese population. Considering the unique social, environmental, and clinical contexts of Chinese patients that may affect psychometric properties, the aim of this study is to translate the ISC-Q into Chinese for cross-cultural adaptation and to evaluate its applicability in a Chinese setting.
To the best of our knowledge, this is the first study in China to investigate the psychometric validity of ISC-Q in NLUTD patients. The significance of this study lies in the localized ISC-Q’s potential to better understand and meet the needs of Chinese patients, bridging the gap between evidence-based recommendations and real-world patient behavior, thereby improving the QOL and treatment outcomes for NLUTD patients.
Methods
Research design and participants
A convenience sampling method was employed in this study. From March 1, 2023, to August 1, 2023, a cross-sectional study was conducted in seven tertiary comprehensive hospitals across China. These hospitals are recognized as critical centers for healthcare, education, and research, each with a minimum of 500 beds.
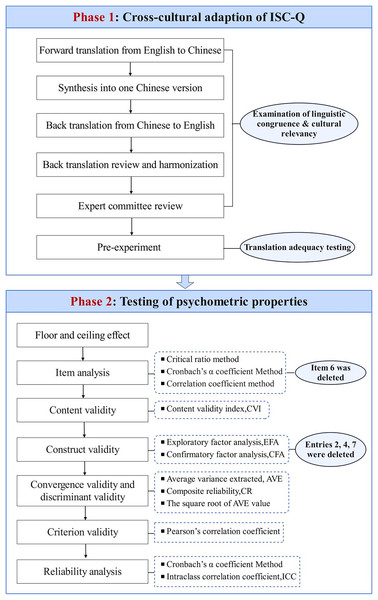
In this study, we utilized the ISC-Q from the PROMs. The ISC-Q is widely recognized as an effective tool within PROMs for assessing the QOL of patients undergoing ISC (Wang et al., 2021a). The investigation was executed in two phases (See Fig. 1): (1) Cross-cultural adaptation to develop the Chinese version of ISC-Q (Beaton et al., 2000; Meng et al., 2023); (2) Psychometric evaluation was conducted following the “Consensus-Based Standards for the Selection of Health Status Measurement Instruments” (COSMIN) checklist (Mokkink et al., 2010; Gagnier et al., 2021).
Figure 1: Process summary of ISC-Q cross-cultural adaptation and psychological test evaluation.
Participants were included based on the following criteria: (1) aged between 18 and 65 years; (2) confirmed diagnosis of NLUTD; (3) prior or current practice of ISC. The exclusion criteria were: (1) cognitive impairments, visual impairments, or hand function impairments; (2) other comorbidities, including urethral stricture, bladder or kidney stones, or rectal dysfunction. To improve the quality and transparency of the research, the team employed the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) Statement checklist (See Appendix 1).
Data collection procedure
The online survey was facilitated through the “Questionnaire Star”, a widely-utilized online platform within the industry. After obtaining consent from specialized incontinence nurses at seven tertiary comprehensive hospitals, the nurses received online training. Upon finalizing the questionnaire’s design, researchers uploaded it to the Questionnaire Star software, generating a unique link. Investigators who completed the training and passed the competency test were officially authorized to conduct the survey.
The researchers distributed the survey link to the principal investigators at each participating center, with a mandate that each center guide a minimum of 60 patients in completing the questionnaire. Specialized incontinence nurses recruited eligible patients in outpatient clinics and provided face-to-face guidance on completing the electronic questionnaire. This ensured that each patient accurately understood the questionnaire content and could complete it independently. Detailed explanations and instructions regarding the study’s purpose, methods, and considerations were provided on the first page of the Questionnaire Star. Each participant had to read and agree to the participation statement before starting the questionnaire, ensuring informed consent and their right to withdraw from the study at any time without adverse consequences. To ensure the quality and completeness of the survey, all questions were mandatory, and respondents were restricted to completing the survey only once from the same IP address. Upon approval from the research team, participants received a compensation of 20 RMB (approximately 3.0 USD).
During data collection, 405 patients from Guangdong, Sichuan, Hubei, and Henan provinces in China were recruited to participate in the survey. After screening out those who refused to participate or completed the questionnaire in less than 420 s, 338 valid questionnaires were obtained, resulting in a response rate of 83.345%. To assess the test-retest reliability of the scale, a follow-up survey link was sent 3 weeks later to participants who agreed to participate again, yielding an additional 30 valid responses.
Sample size calculation
According to the Kendall sample estimation method, the sample size should be 5–10 times the number of questionnaire items (Cong et al., 2020). Given that the ISC-Q has 24 items, the minimum sample size was set at 120. To ensure the randomness and representativeness of the sample, the seven hospitals were sequentially numbered from 1 to 7, followed by the use of a random number generator (such as https://www.random.org/sequences/) to generate a random sequence of these seven numbers. Following this random sequence, we extracted samples from each hospital until the accumulated sample size exceeded the minimum required for exploratory factor analysis (EFA) (See Appendix 2). The remaining samples were used for confirmatory factor analysis (CFA), ensuring that the CFA sample size reached at least 200 (Li, 2016).
Instruments
Socio-demographic and clinical characteristics
Self-designed questionnaires were used to collect sociodemographic and clinical characteristic data.
ISC-Q
The ISC-Q was meticulously developed by Pinder et al. (2012), drawing from an extensive literature review and qualitative studies. This tool was rigorously validated in a cohort of 308 patients with neurogenic bladder disorders (Pinder et al., 2012). Designed for completion by ISC patients, the questionnaire aims to evaluate the QOL related to their unique needs, encompassing both physical and psychological concerns. The ISC-Q comprises 24 items, organized into four dimensions. Each item pertains to the usage of the current type of catheter, providing insights into patients’ perceptions of the device’s benefits and challenges. A five-point Likert scale, ranging from 0 (strongly disagree) to 4 (strongly agree), is employed. After converting responses from 14 reverse-coded items, scores are calculated by averaging the items within each dimension and then multiplying by 25, yielding a universal range of 0–100. The overall ISC-Q score is derived from the mean values across the four dimensions, with a higher ISC-Q score indicating a more favorable QOL in relation to ISC.
Intermittent catheterization acceptance test
The Intermittent catheterization acceptance test (I-CAT), developed by Guinet-Lacoste et al. (2017), consists of 14 items, rated on a five-point Likert scale ranging from 0 (strongly disagree) to 4 (strongly agree). The total score is calculated by summing the responses to 13 items, assessing the level of patient acceptance of ISC. A higher total score on the I-CAT indicates greater acceptance of ISC. The Chinese version of I-CAT was utilized in this study, demonstrating good reliability and validity (Wang et al., 2021b).
Phase I: cross-cultural adaptation of ISC-Q
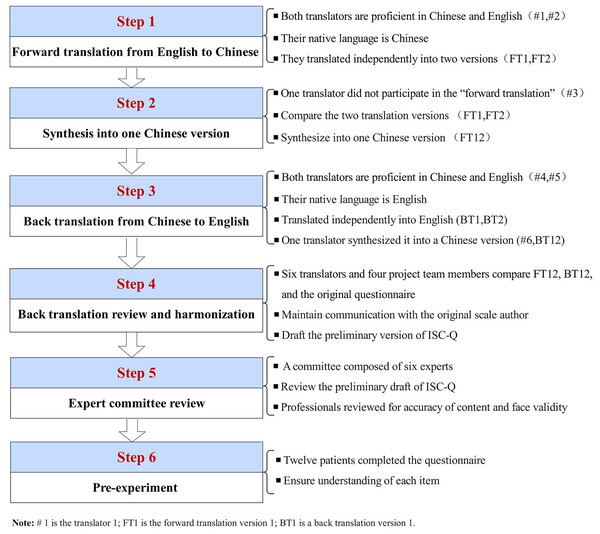
Following obtaining permission and authorization from the original authors through email (Pinder et al., 2012), the ISC-Q underwent cross-cultural adaptation, as outlined in Fig. 2 (Beaton et al., 2000; Meng et al., 2023).
Figure 2: Flowchart of the translation and cross-cultural adaptation process of ISC-Q from the original English version.
Phase II: psychometric evaluation of ISC-Q
Floor and ceiling effects
Floor and ceiling effects were evaluated by btaining the lowest or highest scores on the ISC-Q. If more than 15% of participants achieve the lowest or highest scores, it is considered that there are no floor or ceiling effects. The presence of these effects indicates limited quality of content validity.
Item analysis
Item analysis assessed the internal consistency and discriminative ability of the questionnaire. The critical ratio method, Cronbach’s alpha coefficient method, and correlation coefficient method were employed to screen items. (1) Critical ratio method: Independent sample t-tests were conducted to examine differences in means between the top 27.0% and bottom 27.0% groups for each item (Cong et al., 2020). (2) Cronbach’s alpha coefficient method: If the removal of a specific item resulted in an increase in Cronbach’s alpha coefficient, consideration was given to its deletion (Zhang, Ge & Rask, 2019). (3) Correlation coefficient method: Items with a correlation coefficient <0.20 were considered for deletion (Zhang, Ge & Rask, 2019). Items failing to meet criteria in two of the above-mentioned methods were deleted.
Content validity
Content validity was assessed using the content validity index (CVI). The CVI is divided into scale level (S-CVI) and item level (I-CVI). An S-CVI > 0.90 and an I-CVI > 0.83 indicate satisfactory content validity (Yusoff, 2019).
Construct validity
The structural validity was assessed using EFA and CFA. The criteria for EFA acceptability included a significant Bartlett’s test of sphericity (P < 0.05) and a Kaiser-Meyer-Olkin (KMO) value > 0.60, indicating suitability for factor analysis. Principal component analysis and varimax rotation were used to extract common factors with eigenvalues greater than 1 (Yu et al., 2021). The criteria for factor extraction and retention were as follows (Schreiber, 2021): (1) each common factor should encompass at least three items; (2) factor loadings > 0.50; (3) eigenvalues > 1.00; (4) items with cross-loadings greater than 0.10 were removed.
Additionally, to thoroughly test the factor structure derived from EFA, it is recommended to use CFA and report fit indices. In this study, model fit was evaluated using the following criteria: Standardized Root Mean Square Residual (SRMR) ≤ 0.08, Root Mean Square Error of Approximation (RMSEA) < 0.10, Chi-square divided by degrees of freedom (χ2/df) ≤ 3.00. Comparative Fit Index (CFI) and Tucker-Lewis Index (TLI) values close to or exceeding 0.9 are generally considered indicative of good fit (Xia & Yang, 2019; Balaban & Bilge, 2021).
Convergent and discriminant validity
Convergent validity at the dimension level of the questionnaire was evaluated by calculating the average variance extracted (AVE) and composite reliability (CR). CR > 0.60 and AVE > 0.36 were considered to be acceptable (Cong et al., 2020). Discriminant validity was assessed through the square root of the AVE values and the correlations among the ISC-Q dimensions. A dimension’s square root of the AVE being higher than its correlation with any other dimension signifies good discriminant validity.
Criterion validity
Using the Chinese version of I-CAT as the criterion measure (Wang et al., 2021b), the product-moment correlation coefficient was calculated between ISC-Q and the criterion questionnaire.
Reliability analysis
The internal consistency reliability of the questionnaire was evaluated using Cronbach’s alpha coefficient, where a value of α > 0.70 is considered acceptable (Taber, 2018). This analysis provides insights into how well the items within each dimension of the ISC-Q are correlated with each other, indicating the reliability of the internal structure. To assess the test-retest reliability and measure the stability of responses over time, the intraclass correlation coefficient (ICC) was computed. An ICC value greater than 0.75 is generally excellent reliability, indicating a reliable measurement over time (Koo & Li, 2016).
Ethics statement
Approval was obtained from the Medical Ethics Committees of Southern Medical University Shenzhen Hospital with approval numbers NYSZYYEC20230031. All participants provided electronic informed consent and voluntarily completed the online survey. Additionally, all information obtained from the participants is strictly confidential and anonymized.
Data analysis
EFA and descriptive statistics were conducted using the SPSS26.0 statistical software (SPSS ver. 26.0, Armonk, NY, USA). CFA was performed using the AMOS26.0 software. Continuous data adhering to a normal distribution were presented as mean ± standard deviation, and comparisons between the two samples were assessed using the two-independent-sample t-test. Non-normally distributed continuous data were presented as median (quartiles), and comparisons between the two samples were conducted using the Mann-Whitney U test. Categorical data were presented as frequencies and percentages (%), with comparisons between the two samples analyzed using the χ2 test. A two-sided P-value was used, and a P-value of <0.05 was considered statistically significant.
Results
Participant characteristics
A total of 405 questionnaires were collected from the seven hospitals. The sample distribution is detailed in Appendix 2. In the EFA, 162 participants were eligible, among which 13 questionnaires were invalid and 15 individuals declined to participate. As a result, a total of 134 participants were included with an effective response rate of 82.72%. In the CFA, 243 participants met the criteria, with 18 invalid questionnaires and 21 refusals to participate. Consequently, 204 participants were included, and the effective response rate was 83.95%. The detailed demographic characteristics of the participants can be found in Table 1, while the ISC-Q item scores are presented in Table 2.
| Characteristics | Whole sample (n = 338) | Sample 1 (n = 134) | Sample 2 (n = 204) | P-value |
|---|---|---|---|---|
| Age, years | 0.296a | |||
| Mean ± SD | 39.77 ± 10.01 | 39.04 ± 10.89 | 40.25 ± 9.39 | |
| Gender (n, %) | 0.699b | |||
| Men | 200 (59.2) | 81 (60.4) | 119 (58.3) | |
| Women | 138 (40.8) | 53 (39.6) | 85 (41.7) | |
| Marital status (n, %) | 0.622b | |||
| Unmarried | 93 (27.5) | 42 (31.4) | 51 (25.0) | |
| Married | 197 (58.3) | 75 (56.0) | 122 (59.8) | |
| Divorced | 39 (11.5) | 14 (10.4) | 25 (12.3) | |
| Widow | 9 (2.7) | 3 (2.2) | 6 (2.9) | |
| Occupation (n, %) | 0.497b | |||
| Unemployed | 171 (50.6) | 65 (48.5) | 106 (51.9) | |
| Farmer | 70 (20.7) | 28 (20.9) | 42 (20.6) | |
| Worker | 29 (8.6) | 8 (6.0) | 21 (10.3) | |
| Staff | 18 (5.3) | 8 (6.0) | 10 (4.9) | |
| Individual proprietor | 10 (3.0) | 5 (3.7) | 5 (2.5) | |
| Others | 40 (11.8) | 20 (14.9) | 20 (9.8) | |
| Family residence (n, %) | 0.288b | |||
| City | 84 (24.8) | 36 (26.9) | 48 (23.5) | |
| Town | 80 (23.7) | 36 (26.9) | 44 (21.6) | |
| Countryside | 174 (51.5) | 62 (46.2) | 112 (54.9) | |
| Personal monthly income, (RMB)c | 0.259a | |||
| Mean ± SD | 1,647.40 ± 2,555.15 | 1,453.44 ± 2,116.13 | 1,774.80 ± 2,804.18 | |
| Education level (n, %) | 0.568b | |||
| Junior high school and below | 188 (55.6) | 79 (59.0) | 109 (53.4) | |
| Secondary vocational school | 76 (22.5) | 26 (19.4) | 50 (24.5) | |
| Junior college | 45 (13.3) | 16 (11.9) | 29 (14.2) | |
| Bachelor’s degree and above | 29 (8.6) | 13 (9.7) | 16 (7.9) | |
| First diagnosis of disease (n, %) | 0.488b | |||
| Spinal cord injury | 248 (73.3) | 91 (67.9) | 157 (76.9) | |
| Multiple sclerosis | 6 (1.8) | 3 (2.2) | 3 (1.5) | |
| Stroke | 4 (1.2) | 2 (1.5) | 2 (0.9) | |
| Cauda equina syndrome | 8 (2.4) | 4 (3.0) | 4 (2.0) | |
| Diabetes | 3 (0.9) | 2 (1.5) | 1 (0.5) | |
| Spina bifida | 46 (13.6) | 21 (15.7) | 25 (12.3) | |
| Parkinson’s disease | 2 (0.6) | 2 (1.5) | 0 (0) | |
| Others | 21 (6.2) | 9 (6.7) | 12 (5.9) | |
| Medical expenses payment method (n, %) | 0.982b | |||
| Self-paid | 136 (40.2) | 54 (40.3) | 82 (40.2) | |
| Medical insurance | 178 (52.7) | 70 (52.3) | 108 (53.0) | |
| Work-related injury insurance | 11 (3.3) | 5 (3.7) | 6 (2.9) | |
| Others | 13 (3.8) | 5 (3.7) | 8 (3.9) | |
| Duration of carrying out ISC, years | 0.830a | |||
| Mean ± SD | 2.97 ± 4.63 | 3.04 ± 4.46 | 2.93 ± 4.75 | |
| Urinary tract infection (n, %) | 0.475b | |||
| 0 times/year | 69 (20.4) | 22 (16.4) | 47 (23.0) | |
| 1–2 times/year | 178 (52.7) | 72 (53.8) | 106 (52.0) | |
| 3–4 times/year | 45 (13.3) | 20 (14.9) | 25 (12.3) | |
| >4 times/year | 46 (13.6) | 20 (14.9) | 26 (12.7) | |
| ISC-Q items | Whole sample (n = 338) | Sample 1 (n = 134) | Sample 2 (n = 204) | P-valuea | |||
|---|---|---|---|---|---|---|---|
| Mean ± SD | Cronbach’s α | Mean ± SD | Cronbach’s α | Mean ± SD | Cronbach’s α | ||
| Ease of use | 67.71 ± 18.52 | 0.780 | 67.30 ± 19.10 | 0.792 | 67.98 ± 18.17 | 0.774 | 0.742 |
| ISCQ1 | 71.06 ± 23.56 | 72.39 ± 23.40 | 70.10 ± 23.68 | 0.383 | |||
| ISCQ3 | 63.83 ± 26.18 | 64.93 ± 25.30 | 63.11 ± 26.78 | 0.534 | |||
| ISCQ5 | 70.12 ± 21.84 | 68.28 ± 22.35 | 71.32 ± 21.46 | 0.211 | |||
| ISCQ8 | 65.90 ± 23.68 | 63.62 ± 26.12 | 67.40 ± 21.85 | 0.151 | |||
| Convenience | 42.97 ± 19.15 | 0.829 | 42.26 ± 21.27 | 0.838 | 43.44 ± 22.65 | 0.825 | 0.630 |
| ISCQ9 | 53.18 ± 27.49 | 52.99 ± 25.84 | 53.31 ± 28.59 | 0.916 | |||
| ISCQ10 | 44.08 ± 27.27 | 42.91 ± 25.21 | 44.85 ± 28.58 | 0.523 | |||
| ISCQ11 | 40.24 ± 28.45 | 37.31 ± 26.15 | 42.16 ± 29.77 | 0.116 | |||
| ISCQ12 | 34.39 ± 25.38 | 35.82 ± 26.45 | 33.46 ± 24.67 | 0.403 | |||
| Discreetness | 59.05 ± 20.24 | 0.861 | 58.64 ± 20.20 | 0.856 | 59.31 ± 20.31 | 0.864 | 0.767 |
| ISCQ13 | 62.94 ± 25.78 | 61.38 ± 26.48 | 63.97 ± 25.32 | 0.367 | |||
| ISCQ14 | 58.14 ± 26.13 | 58.02 ± 26.48 | 58.21 ± 25.97 | 0.948 | |||
| ISCQ15 | 58.51 ± 26.40 | 58.96 ± 25.36 | 58.21 ± 27.13 | 0.800 | |||
| ISCQ16 | 63.02 ± 26.63 | 62.87 ± 27.20 | 63.11 ± 26.31 | 0.936 | |||
| ISCQ17 | 55.99 ± 25.97 | 55.04 ± 25.61 | 56.62 ± 26.24 | 0.585 | |||
| ISCQ18 | 55.70 ± 27.22 | 55.60 ± 27.87 | 55.76 ± 26.85 | 0.957 | |||
| Psychological well-being | 37.11 ± 19.66 | 0.863 | 36.94 ± 20.73 | 0.886 | 37.21 ± 18.97 | 0.846 | 0.901 |
| ISCQ19 | 46.67 ± 27.74 | 45.52 ± 28.57 | 47.42 ± 27.23 | 0.538 | |||
| ISCQ20 | 37.72 ± 26.21 | 36.57 ± 25.59 | 38.48 ± 26.65 | 0.512 | |||
| ISCQ21 | 37.50 ± 25.42 | 36.94 ± 24.85 | 37.86 ± 25.85 | 0.743 | |||
| ISCQ22 | 34.02 ± 23.74 | 34.70 ± 24.70 | 33.57 ± 23.14 | 0.671 | |||
| ISCQ23 | 36.83 ± 26.49 | 35.82 ± 26.45 | 37.50 ± 26.55 | 0.569 | |||
| ISCQ24 | 29.88 ± 23.24 | 32.09 ± 25.58 | 28.43 ± 21.50 | 0.172 | |||
| ISC-Q | 50.98 ± 12.30 | 0.821 | 50.59 ± 12.77 | 0.837 | 51.24 ± 12.00 | 0.809 | 0.632 |
Notes:
Abbreviation: SD, standard deviation; ISC-Q, Intermittent self-catheterization questionnaire.
Phase I: translation and cross-cultural adaptation process
The formulation of the simplified Chinese version of ISC-Q involved expert consultations. Andrew J. Lloyd, the original questionnaire author, provided invaluable suggestions and comments. While the original questionnaire format was retained, certain modifications were introduced to improve clarity and understanding. For instance, the phrase “due to the lubricant” was incorporated into item 2, “for example, catheterizing in public restrooms” was appended to item 16, and in item 17, “discreet” was substituted with “inconspicuous” and further elucidated as “not easily noticed or seen by others”. All modifications underwent validation by a panel of ten experts, with the finalized version of ISC-Q available in Appendix 3. The content validity S-CVI stood at 0.967, and the derived I-CVI values ranged between 0.800 and 1.00, reflecting strong content validity (Yusoff, 2019).
Phase II: psychometric evaluation of ISC-Q
Floor and ceiling effects and item analysis
No floor or ceiling effects were detected. The independent sample t-test result for item 6 was not significant (P > 0.05). The item-total correlation coefficient for item 6 was r = 0.132, which is less than 0.2 (P > 0.05). Additionally, if item 6 were removed, the Cronbach’s α coefficient would increase. Therefore, item 6 was excluded (See Table 3).
| ISC-Q items | Critical ration t | P-value | Item-to-total correlations | Cronbach’s α if item deleted | Floor effects (n, %) | Ceiling effects (n, %) |
|---|---|---|---|---|---|---|
| Ease of use | 2 (1.5) | 0 (0) | ||||
| ISCQ1 | −4.089 | <0.001 | 0.316*** | 0.836 ↓ | ||
| ISCQ2 | −3.131 | 0.003 | 0.378*** | 0.834 ↓ | ||
| ISCQ3 | −6.842 | <0.001 | 0.534*** | 0.828 ↓ | ||
| ISCQ4 | −2.768 | 0.007 | 0.260** | 0.838 ↓ | ||
| ISCQ5 | −4.043 | <0.001 | 0.314*** | 0.836 ↓ | ||
| ISCQ6 | −1.686 | 0.096 | 0.132 | 0.841 ↑ | ||
| ISCQ7 | −3.260 | 0.002 | 0.418*** | 0.833 ↓ | ||
| ISCQ8 | −5.297 | <0.001 | 0.482*** | 0.830 ↓ | ||
| Convenience | 2 (1.5) | 5 (3.7) | ||||
| ISCQ9 | −4.117 | <0.001 | 0.436*** | 0.832 ↓ | ||
| ISCQ10 | −5.219 | <0.001 | 0.561*** | 0.826 ↓ | ||
| ISCQ11 | −5.559 | <0.001 | 0.558*** | 0.827 ↓ | ||
| ISCQ12 | −5.355 | <0.001 | 0.598*** | 0.825 ↓ | ||
| Discreetness | 9 (6.7) | 1 (0.7) | ||||
| ISCQ13 | −5.303 | <0.001 | 0.397*** | 0.834 ↓ | ||
| ISCQ14 | −5.143 | <0.001 | 0.438*** | 0.832 ↓ | ||
| ISCQ15 | −2.671 | 0.007 | 0.279** | 0.838 ↑ | ||
| ISCQ16 | −5.062 | <0.001 | 0.461*** | 0.831 ↓ | ||
| ISCQ17 | −4.768 | <0.001 | 0.416*** | 0.833 ↓ | ||
| ISCQ18 | −4.024 | <0.001 | 0.413*** | 0.833 ↓ | ||
| Psychologicalwell-being | 2 (1.5) | 9 (6.7) | ||||
| ISCQ19 | −5.569 | <0.001 | 0.566*** | 0.826 ↓ | ||
| ISCQ20 | −5.534 | <0.001 | 0.571*** | 0.826 ↓ | ||
| ISCQ21 | −6.081 | <0.001 | 0.629*** | 0.824 ↓ | ||
| ISCQ22 | −4.410 | <0.001 | 0.540*** | 0.827 ↓ | ||
| ISCQ23 | −6.113 | <0.001 | 0.603*** | 0.824 ↓ | ||
| ISCQ24 | −5.114 | <0.001 | 0.595*** | 0.825 ↓ | ||
| ISC-Q | 0 (0) | 0 (0) | ||||
| Cronbach’s α | 0.837 | |||||
Notes:
Item-to-Total Correlations using Pearson’s correlation test; Items that are deleted are displayed in bold; The symbol “↓” indicates that if the item is removed, the Cronbach’s α coefficient would decrease.
Abbreviation: ISC-Q, Intermittent self-catheterization questionnaire.
EFA
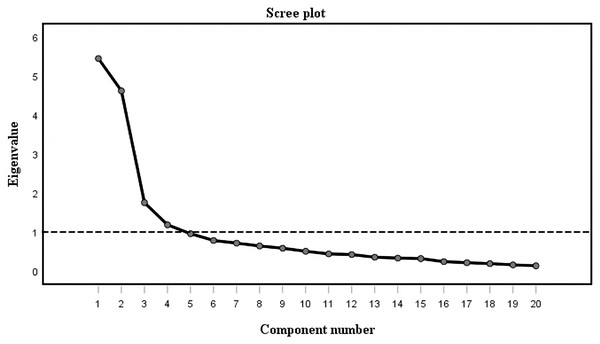
The Kaiser-Meyer-Olkin (KMO) measure yielded a value of 0.812, and the Bartlett’s test of sphericity was significant with a statistic of 1,632.200 (χ2 = 1,632.200, df = 253, P < 0.001), suggesting the sample data was suitable for EFA. The initial EFA indicated five factors with eigenvalues exceeding 1.0; however, one factor contained less than two items (items 2 and 4), and based on criteria stipulating at least three items per factor, it was removed. The subsequent EFA revealed four factors, but item 7 was discarded due to a factor loading less than 0.5. The final EFA extracted four factors encompassing 20 items with factor loadings ranging from 0.588 to 0.872. These factors were labeled based on content characterization: Ease of Use (Factor 1), Convenience (Factor 2), Discreetness (Factor 3), and Psychological Well-being (Factor 4), accounting for 64.953% of the total variance (See Table 4). The scree plot further elucidated the factor structure, indicating a subtle decline after the fourth point (See Fig. 3).
| Item number and description | Factor load after rotation (n = 134) | Test–retest reliability (n = 25) | |||||
|---|---|---|---|---|---|---|---|
| Factor-1 | Factor-2 | Factor-3 | Factor-4 | ICC | 95% CI | P-value | |
| Ease of use | |||||||
| ISCQ1: It is easy to prepare my catheter for use each time I need it. | 0.829 | 0.107 | 0.045 | 0.078 | 0.722 | [0.493–0.857] | <0.001 |
| ISCQ3: It is easy to insert my catheter. | 0.789 | −0.035 | 0.310 | 0.159 | 0.858 | [0.723–0.930] | <0.001 |
| ISCQ5: The design of the catheter makes it easy to insert. | 0.595 | −0.138 | 0.244 | −0.015 | 0.840 | [0.691–0.921] | <0.001 |
| ISCQ8: I feel confident in my ability to use my catheter. | 0.726 | −0.142 | 0.355 | 0.119 | 0.793 | [0.610–0.896] | <0.001 |
| Convenience | |||||||
| ISCQ9: Storage of catheters at home is inconvenienta. | 0.059 | 0.696 | −0.217 | 0.307 | 0.803 | [0.627–0.901] | <0.001 |
| ISCQ10: Taking enough catheters for a weekend away is very inconvenienta. | −0.064 | 0.788 | 0.059 | 0.373 | 0.781 | [0.590–0.889] | <0.001 |
| ISCQ11: Taking enough catheters for a 2-week holiday is very inconvenienta. | −0.160 | 0.719 | 0.175 | 0.396 | 0.861 | [0.729–0.931] | <0.001 |
| ISCQ12: Disposal of my catheter is inconvenient when away from homea. | −0.095 | 0.588 | 0.161 | 0.500 | 0.673 | [0.418–0.830] | <0.001 |
| Discreetness | |||||||
| ISCQ13: I find it easy to carry enough catheters around with me on a day-to-day basis. | 0.262 | 0.233 | 0.644 | −0.136 | 0.733 | [0.511–0.863] | <0.001 |
| ISCQ14: I find it easy to dispose of my catheter when l am away from home. | 0.091 | 0.113 | 0.824 | −0.036 | 0.695 | [0.451–0.842] | <0.001 |
| ISCQ15: My catheter is inconspicuous (not easily noticed). | 0.174 | −0.045 | 0.732 | −0.151 | 0.686 | [0.438–0.837] | <0.001 |
| ISCQ16: I can use my catheter discreetly when l am away from home. | 0.105 | 0.004 | 0.837 | 0.044 | 0.737 | [0.517–0.866] | <0.001 |
| ISCQ17: I can easily dispose of my catheter without it being obvious to people. | 0.246 | −0.021 | 0.760 | −0.005 | 0.762 | [0.559–0.879] | <0.001 |
| ISCQ18: My catheter allows me to feel confident when away from home. | 0.195 | −0.337 | 0.619 | 0.215 | 0.664 | [0.405–0.825] | <0.001 |
| Psychological well-being | |||||||
| ISCQ19: I am self-conscious about my need to self-catherizea. | 0.028 | 0.232 | −0.095 | 0.745 | 0.787 | [0.600–0.893] | <0.001 |
| ISCQ20: I would feel embarrassed if people saw my catheter in its packeta. | −0.019 | 0.099 | 0.034 | 0.792 | 0.711 | [0.475–0.851] | <0.001 |
| ISCQ21: My need to use a catheter sometimes makes me feel embarrasseda. | 0.112 | 0.119 | −0.124 | 0.872 | 0.781 | [0.589–0.889] | <0.001 |
| ISCQ22: I worry that my catheter doesn’t always empty my bladder fullya. | 0.084 | 0.327 | −0.138 | 0.672 | 0.809 | [0.637–0.904] | <0.001 |
| ISCQ23: My need to use catheters stops me from visiting friends and family as often as I would likea. | 0.051 | 0.195 | 0.057 | 0.732 | 0.830 | [0.673–0.915] | <0.001 |
| ISCQ24: I worry about the risk of long-term problems from using my cathetera. | −0.056 | 0.194 | 0.046 | 0.783 | 0.734 | 0.512–0.864] | <0.001 |
| ISC-Q | 0.951 | [0.900–0.976] | <0.001 | ||||
| % of the variance | 21.593 | 18.665 | 12.376 | 12.319 | |||
| Cumulative variance (%) | 21.593 | 40.258 | 52.634 | 64.953 | |||
Notes:
Extraction method (Principal Component Analysis); Rotation method (Oblimin with Kaiser Normalization); Factors > 0.4 are shown in bold.
Abbreviation: CI, Confidence interval; ICC, Intraclass correlation coefficient; ISC-Q, Intermittent self-catheterization questionnaire.
Figure 3: Scree plot for ISC-Q.
Note: The scree plot was acquired by principal component analysis with correlation matrix. Component number 4 is the elbow point and its eigenvalue is >1. Thus, four factors were extracted.CFA
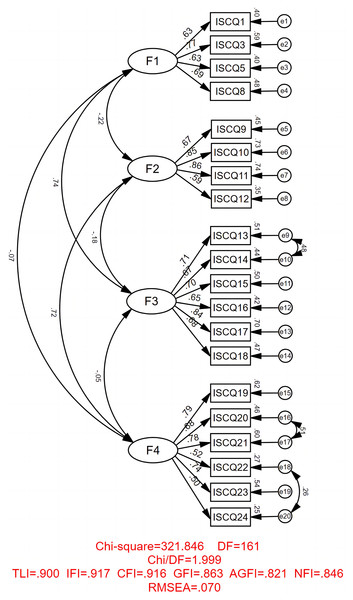
The CFA further validated the four-factor structure derived from EFA. All items demonstrated statistically significant factor loadings on their respective latent factors (P < 0.001), with loadings ranging from 0.496 to 0.860. Three residual covariances: cov (e9, e10); cov (e16, e17); and cov (e18, e20) were set as free parameters to enhance model fit. The fit indices were as follows: χ2 = 321.846, χ2/df = 1.999, GFI = 0.863, AGFI = 0.821, SRMR = 0.076, RMSEA = 0.070; TLI = 0.900, IFI = 0.917, and CFI = 0.916, suggesting a satisfactory fit for the model (See Fig. 4). Furthermore, cross-validation was performed, confirming the four-factor structure elucidated in the analyses (See Table 5). Comparative analysis with other models demonstrated deterioration in fit indices. A chi-square test at a significance level of 0.001 further indicated the superior fit of the original model.
Figure 4: Fitting figure of modification model of the revised 20-item Chinese version of ISC-Q.
Note: The squares represent the item; the oval features represent the factor1-factor 4; F1 (Ease of use); F2 (Convenience); F3 (Discreetness); F4 (Psychological well-being); the small ovals were the error terms; all estimates are statistically significant (<0.001).| Number | Model | χ2 | df | χ2/df | NFI | CFI | RMSEA | Model comparison | Δχ2 | Δ df | P-value |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | Original model | 321.846 | 161 | 1.999 | 0.846 | 0.916 | 0.070 | ||||
| 2 | Three-factor model I | 600.190 | 164 | 3.660 | 0.713 | 0.771 | 0.114 | 2 vs. 1 | 278.344 | 3 | <0.001 |
| 3 | Three-factor model II | 718.086 | 164 | 4.379 | 0.657 | 0.709 | 0.129 | 3 vs. 1 | 396.240 | 3 | <0.001 |
| 4 | Three-factor model III | 797.204 | 164 | 4.861 | 0.619 | 0.668 | 0.138 | 4 vs. 1 | 475.358 | 3 | <0.001 |
| 5 | Two-factor model | 774.945 | 166 | 4.668 | 0.630 | 0.680 | 0.134 | 5 vs. 1 | 453.099 | 5 | <0.001 |
| 6 | Single-factor model | 1,050.264 | 167 | 6.289 | 0.499 | 0.536 | 0.161 | 6 vs. 1 | 728.418 | 6 | <0.001 |
Notes:
Best-fitting model is highlighted in boldface; df, degrees of freedom; NFI, normed fit index; CFI, comparative fit index; RMSEA, root mean square error of approximation; Δχ2, chi-square difference test; Three-factor model I (F1 + F2, F3, F4); Three-factor model II (F1, F2 + F3, F4); Three-factor model III (F1, F2, F3 + F4); Two-factor model (F3, F4); Single-factor model (F4).
Abbreviation: ISC-Q, Intermittent self-catheterization questionnaire.
Convergent validity
The AVE for these factors was between 0.466 and 0.565. With CR values ranging from 0.776 to 0.859, all exceeding the 0.7 threshold, the results suggest good convergent validity for the Chinese version of the ISC-Q (Cong et al., 2020) (See Table 6).
| Path analysis | Unstandardized factor loading | Standardized factor loading | SE | P-value | AVE | CR | The square root of AVE | |
|---|---|---|---|---|---|---|---|---|
| Ease of use | 0.466 | 0.776 | 0.683 | |||||
| ISCQ1 | <---F1 | 1 | 0.629 | |||||
| ISCQ3 | <---F1 | 1.382 | 0.769 | 0.164 | <0.001 | |||
| ISCQ5 | <---F1 | 0.909 | 0.631 | 0.128 | <0.001 | |||
| ISCQ8 | <---F1 | 1.015 | 0.692 | 0.139 | <0.001 | |||
| Convenience | 0.565 | 0.835 | 0.752 | |||||
| ISCQ9 | <---F2 | 1 | 0.668 | |||||
| ISCQ10 | <---F2 | 1.277 | 0.853 | 0.130 | <0.001 | |||
| ISCQ11 | <---F2 | 1.342 | 0.860 | 0.134 | <0.001 | |||
| ISCQ12 | <---F2 | 0.761 | 0.588 | 0.102 | <0.001 | |||
| Discreetness | 0.506 | 0.859 | 0.711 | |||||
| ISCQ13 | <---F3 | 1 | 0.712 | |||||
| ISCQ14 | <---F3 | 0.961 | 0.667 | 0.079 | <0.001 | |||
| ISCQ15 | <---F3 | 1.060 | 0.704 | 0.116 | <0.001 | |||
| ISCQ16 | <---F3 | 0.947 | 0.649 | 0.111 | <0.001 | |||
| ISCQ17 | <---F3 | 1.220 | 0.838 | 0.117 | <0.001 | |||
| ISCQ18 | <---F3 | 1.016 | 0.682 | 0.117 | <0.001 | |||
| Psychological well-being |
0.459 | 0.831 | 0.677 | |||||
| ISCQ19 | <---F4 | 1 | 0.790 | |||||
| ISCQ20 | <---F4 | 0.841 | 0.678 | 0.091 | <0.001 | |||
| ISCQ21 | <---F4 | 0.934 | 0.777 | 0.086 | <0.001 | |||
| ISCQ22 | <---F4 | 0.563 | 0.523 | 0.080 | <0.001 | |||
| ISCQ23 | <---F4 | 0.911 | 0.738 | 0.090 | <0.001 | |||
| ISCQ24 | <---F4 | 0.496 | 0.496 | 0.075 | <0.001 | |||
Notes:
F1 (Ease of use); F2 (Convenience); F3 (Discreetness); F4 (Psychological well-being).
Abbreviation: AVE, average variance extracted, CR, composite reliability, SE, standard error; ISC-Q, Intermittent self-catheterization questionnaire.
Discriminant validity
The dimension “Ease of Use” displayed no significant correlation with “Convenience” (P > 0.001) but exhibited a highly significant positive correlation with “Discreetness” (P < 0.001, r = 0.744). “Convenience” demonstrated a significant positive correlation with “Psychological Well-being” (P < 0.001, r = 0.720) but showed no association with “Discreetness”. “Psychological Well-being” had no discernible relationship with either “Ease of Use” or “Discreetness” (P > 0.001) (See Fig. 4). Crucially, the square root of the AVE for each dimension surpassed the correlation coefficients between that dimension and others, affirming the questionnaire’s robust discriminant validity (See Table 6).
Criterion validity
The correlation between ISC-Q scores and I-CAT scores was examined using Pearson correlation analysis. The results showed that scores from the Chinese version of ISC-Q showed a strong and statistically significant positive correlation with scores from I-CAT (r = 0.557, P < 0.001). This suggests that as the QOL related to ISC improves, patients are more inclined to accept ISC.
Reliability analysis
The Chinese version of ISC-Q demonstrated excellent internal consistency, with a Cronbach’s α coefficient of 0.821 for the entire questionnaire. The Cronbach’s α coefficients for the four factors were 0.780, 0.829, 0.861, and 0.863, respectively (See Table 2). Additionally, the ICC for the questionnaire was 0.951 (95% CI [0.900–0.976]; P < 0.001) (See Table 4), indicating that the instrument’s stability was deemed acceptable in this study.
Discussion
The study’s findings indicate that ISC-Q exhibits sufficient validity (structural, convergent, discriminant, and criterion-related validity), satisfactory reliability (internal consistency and test-retest reliability), and no floor or ceiling effects.
Upon verifying that the dataset met the necessary assumptions, this study robustly evaluated factor validity through EFA and CFA on two independent samples. The findings indicated that factor loadings in both samples exceeded 0.5, signifying that the correlation between measurement variables (i.e., item scores and factor scores) ranged from good to excellent (Finch, 2020). Furthermore, both EFA and CFA results corroborated the four-factor structure proposed in the original study, collectively accounting for 64.953% of the total variance, substantially surpassing the 49% in the prior research (Pinder et al., 2012). However, this study observed a reduction in the number of items in the “Ease of Use” dimension compared to the original, eliminating “Items 2, 4, 6, and 7”. This alteration might stem from two factors: first, the challenge of comprehending and responding to these reversed items for participants with lower education levels (55.6%, with education up to junior high school); second, the longer duration of ISC use among patients in this study (average 2.97 ± 4.63 years), possibly leading to desensitization to items describing difficulties in ISC (Joshi et al., 2022). These distinctive findings suggest that, compared to other countries, Chinese patients have unique perspectives and experiences regarding QOL associated with ISC.
In this study, we chose the I-CAT as the criterion for criterion validity, diverging from the standards used in previous research (Pinder et al., 2012; Yoshida et al., 2017; Yeşil et al., 2020). This decision was primarily influenced by two considerations: Firstly, one of the main objectives of assessing the QOL of NLUTD patients undergoing ISC is to provide a basis for targeted interventions, thereby increasing patient acceptance of ISC. Secondly, the criterion validity standards employed in other studies have not undergone cross-cultural adaptation and psychometric validation in China. The findings revealed a significant moderate positive correlation between the total ISC-Q score and I-CAT scores (r = 0.557, P < 0.05), indicating acceptable criterion validity. This suggests that higher ISC-related QOL scores in patients correspond to increased acceptance of ISC, consistent with findings in other research (Seth, Haslam & Panicker, 2014; Gharbi et al., 2022). This further implies that enhancing the QOL of NLUTD patients undergoing ISC can help reduce negative emotions and experiences caused by various factors, thereby strengthening the patients’ willingness and motivation to adhere to the ISC treatment regimen (Seth, Haslam & Panicker, 2014; Joshi et al., 2022).
Regarding reliability, the Cronbach’s alpha coefficient for the entire scale, subscales, and individual items exceeded 0.7, indicating that the internal consistency of the ISC-Q is acceptable (Taber, 2018), albeit slightly lower than in previous studies (Pinder et al., 2012; Yoshida et al., 2017; Yeşil et al., 2020). This difference might relate to item deletion and the characteristics of the sample. The ICC for the total questionnaire obtained within 3 weeks in this study was 0.951, nearly identical to the results of Yeşil et al. (2020) (ICC = 0.947), and higher than the original study (ICC = 0.848) (Pinder et al., 2012). This conclusively demonstrates the good stability of the Chinese version of the ISC-Q.
The results of this study reveal a relatively lower QOL among Chinese patients with NLUTD undergoing ISC. Specifically, the average ISC-Q score in this study was 50.98 (out of a maximum 100 points, equivalent to 50.98% of the scoring criteria), markedly lower than the score range in other countries (53.5% to 69%) (Yoshida et al., 2017; Scivoletto et al., 2017; Yeşil et al., 2020). This disparity can be interpreted from several perspectives. First, different cultural backgrounds may largely explain this variance. Additionally, the removal of four items from the original ISC-Q (Pinder et al., 2012) in this study might have influenced the outcomes. Another plausible factor to consider is the sample characteristics. Our findings suggest that a universally lower QOL may be prevalent among ISC patients in China and other cultural contexts. Thus, medical professionals should recognize that a low QOL is not merely unique to certain patients or cultural backgrounds but is a broader issue. In light of this, a thorough assessment of the QOL of ISC patients is particularly crucial. Moreover, it’s noteworthy that, compared to other studies (Pinder et al., 2012; Yoshida et al., 2017; Scivoletto et al., 2017; Yeşil et al., 2020), participants in this study scored particularly poorly in the psychological health dimension, highlighting the need for medical teams to pay more attention to the psychological well-being of patients in daily practice.
Despite these strengths, this study has the following limitations: In this study, the data collection method relies on patients’ self-reported outcomes, which may be subject to personal biases. Furthermore, the cross-sectional design of the study precludes interpretations of causal relationships between variables. Finally, a convenience sampling method was used in this study. Although multiple hospitals were selected to enhance the sample’s representativeness, this limitation still persists. Future research is recommended to employ more rigorous random sampling methods to reduce sampling bias and enhance the external validity of the findings.
Conclusions
After undergoing a rigorous process of cross-cultural debugging and validation, it has been demonstrated for the first time that the Chinese version of ISC-Q is effective and reliable. Furthermore, it exhibits excellent psychometric properties and can be employed to assess the QOL of NLUTD patients undergoing ISC.
The findings of this study unveil a rather pessimistic scenario regarding the QOL of NLUTD patients practicing ISC. In future clinical practice, this tool can be utilized to assist healthcare professionals in identifying the obstacles and challenges faced by NLUTD patients. It can guide them in providing targeted interventions to bridge the gap between evidence-based recommendations and real-world patient behavior. Furthermore, the use of the ISC-Q tool in future research can investigate the interplay between ISC-Q scores, ISC satisfaction, and compliance.