Effects of different ablation points of renal denervation on the efficacy of resistant hypertension
- Published
- Accepted
- Received
- Academic Editor
- Tao Lu
- Subject Areas
- Cardiology, Neurology, Surgery and Surgical Specialties, Urology
- Keywords
- Ablation points, Resistant hypertension
- Copyright
- © 2020 Zhang et al.
- Licence
- This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits using, remixing, and building upon the work non-commercially, as long as it is properly attributed. For attribution, the original author(s), title, publication source (PeerJ) and either DOI or URL of the article must be cited.
- Cite this article
- 2020. Effects of different ablation points of renal denervation on the efficacy of resistant hypertension. PeerJ 8:e9842 https://doi.org/10.7717/peerj.9842
Abstract
Objective
To explore the blood pressure response to different ablation points of renal denervation (RDN) in patients with resistant hypertension
Methods
A total of 42 cases with resistant hypertension treated by RDN in our center from 2013 to 2015 were retrospectively analyzed. The patients were divided into two groups according to the different ablation points of RDN: the standard treatment group (spiral ablation from near to proximal, with less than 8 points per artery) and the intensive treatment group (from near to far by spiral ablation, with at least 8 points per artery), with 21 patients in each group. The ablation parameters, including points, impedance, actual wattage, and actual temperature, were recorded intraoperatively. Renal angiography was performed again after RDN. Ambulatory blood pressure (ABP) images were taken for all patients at the baseline and 6 months after operation.
Results
The mean 24-h blood pressure of the standard treatment group was lower than that of the baseline (24-h systolic blood pressure decreased by 7.4 ± 10.6 mmHg and 24-h diastolic blood pressure decreased by 4.6 ± 6.1 mmHg), and the mean 24-h blood pressure decreased significantly from baseline to 6 months in the intensive treatment group (24–h systolic blood pressure decreased by 27.4 ± 11.4 mmHg, P < 0.0001; 24–h diastolic blood pressure decreased by 10.9 ± 9.6 mmHg, P = 0.005). There was a positive correlation between the decrease of systolic/diastolic 24-hour mean and the number of ablation points used in the procedure. The mean value of systolic and diastolic blood pressure was positively correlated with ablation points at 24-hour (R2 = 0.777 and 0.633 respectively, P < 0.01). There were no adverse events in either group after the operation and during the follow-up.
Conclusions
RDN could significantly reduce BP in patients with resistant hypertension. Our study showed that the antihypertensive effect appeared to be positively correlated with the number of ablation points.
Introduction
Hypertension is the most common risk factor for increased morbidity and mortality for cardiovascular diseases (Fagard, 2012). Although the general tolerability of drug treatment is good, about 10–20% of resistant hypertension drug treatment is ineffective (Dudenbostel et al., 2017). Patients with resistant hypertension have a worse cardiovascular disease prognosis, including coronary heart disease, stroke, chronic heart failure, peripheral artery disease, and chronic kidney disease, compared to patients with more easily controlled hypertension (Sim et al., 2015; Thomas et al., 2016). In the past decade, several studies have shown that percutaneous renal denervation (RDN) blocks the sympathetic adrenergic system and the renin-angiotensin system by applying radiofrequency energy directly in the renal artery wall (Krum et al., 2014; Symplicity HTN-2 Investigators et al., 2010; Davis et al., 2013; Atherton, Deep & Mendelsohn, 2012; DiBona, 2003). RDN reduces water and sodium retention and renin release, and increases renal blood flow, implying that it can be a potential treatment for refractory hypertension (Davis et al., 2013; Atherton, Deep & Mendelsohn, 2012; DiBona, 2003). Despite the promising data from earlier clinical studies, the results of the Symplicity HTN-3 trial showed no significant difference between the RDN group and the sham-treated patients (Bhatt, Kandzari & O’Neill, 2014). However, this may be due to the discontent drug dependence, disadvantageous patient choice, or the restriction of therapy techniques. The latter includes the potentially incomplete or insufficient ablation because the number of ablation sites is small, especially in patients who received complete ablation (Kandzari et al., 2015). Results from recent studies supported this hypothesis, which showed reduced release of norepinephrine by co-ablating the primary renal artery and its branches, suggesting that increasing the number of ablation points and altering the ablation sites may have superimposed effects (Henegar et al., 2015; Fengler et al., 2017). In light of these observations, the present study used retrospective analysis to evaluate the antihypertensive effect of RDN on refractory hypertension and the correlation between different ablation points and antihypertensive efficacy.
Methods
Patient selection and follow-up
In this retrospective study, all patients who received RDN were above 18 years old and complied with the European Consensus 12. The detailed inclusion criteria were: (1) patients have been treated with three or more antihypertensive drugs, including a diuretic (During the study, there was no change in the treatment of hypertension.); (2) the mean of 24-hour systolic BP>140 mmHg (Calhoun et al., 2008) ; and (3) the estimated glomerular filtration rate (eGFR) ≥45 mL/min/1.73 m2 during hospitalization. In addition, patients were excluded if they showed any contraindications to RDN, or displayed any signs of the following conditions: (1) mental illness; (2) pregnancy or contraception; (3) allergic to iodine-containing rays and contrast media; (4) secondary hypertension (renal artery stenosis, coarctation of aorta, hyperaldosteronism, hyperthyroidism and pheochromocytoma); (5) malignant diseases; (6) New York Heart Association class III-IV with congestive heart failure; (7) hypertensive heart failure; (8) chronic renal failure 4–5 (eGFR ≤30 mL/min/1.73 m2); (9) arrhythmia (II degree, III degree atrioventricular block or sinus bradycardia<40 bpm); and (10) valvular disease. Patients were excluded from the study if they had a change in drug use. The study was approved by the Institutional Ethics Committee of Putuo Hospital, Shanghai University of Traditional Chinese Medicine (# 002192).
Ambulatory blood pressure measurement
Ambulatory BP measurement (ABPM) was evaluated with a cuff-based oscillometric device at baseline and 6 months post operation. BP recording was performed every 15 min during the day (7:00 AM to 10:00 PM) and every 30 min during the night (10:00 PM to 7:00 AM) according to the latest European Society of Cardiology guidelines (Calhoun et al., 2008).
Renal denervation
All patients were premedicated by intaking enteric-coated aspirin or 300-mg Clopidogrel hydrogen sulfate tablets. Both renal arteries were ablated using the Symplicity RDN System (Boston Scientific, St. Paul, Minnesota, USA and IBI, St. Jude Medical Systems, Inc.) via transfemoral access. Catheter tip temperature and impedance were monitored during ablation with the temperature fluctuating between 28−35 °C. The energy was between 6–14 W with ablation for 60 s at each point. Depending on the renal artery, the anatomical ablation was performed with a maximum of 16 points in the right and left renal arteries. Pain was relieved by intravenous injection of remifentanil or morphine for all the patients. All procedures were performed by experienced interventional cardiologists.
Safety assessment
The biochemical index, ABPM and transthoracic echocardiography were performed, and eGFR were assessed before RDN and after 6 months for both groups.
Statistical analyses
Quantitative data was presented as mean ± SD and categorical data were presented using counts and percentages. Group comparisons were made by using independent two-sample t-test for continuous data and Chi-square test or Fisher exact test for categorical data, as appropriate. Spearman correlation coefficient was used to evaluate the correlation between parameters. P < 0.05 was considered statistically significant. All data was analyzed using SPSS version 22.0 software (IBM Corp., Armonk, NY, USA).
| Index | Standard treatment | Intensive treatment | P |
|---|---|---|---|
| n (%) | 21 (50.0) | 21 (50.0) | 1.00 |
| Age, y | 61.8 ± 13.3 | 62.7 ± 12.8 | .713 |
| Sex (male), n(%) | 16 (38.1) | 15 (35.7) | .726 |
| HR (bpm, ) | 79.7 ± 10.0 | 82.0 ± 17.0 | .612 |
| Medical history n(%) | |||
| CAD | 6 (14.4) | 10 (24.0) | .170 |
| 2-DM | 9 (23.8) | 9 (23.8) | .622 |
| Atrial fibrillation | 3 (7.1) | 0 (0.0) | .116 |
| Hyperlipidemia | 3 (7.1) | 4 (9.5) | .500 |
| Stroke | 4 (9.5) | 1 (2.4) | .172 |
| Type of antihypertensive medication n(%) | |||
| RAAS Blockers | 20 (48.0) | 13 (31.2) | .010 |
| β-Blocker | 18 (43.2) | 14 (33.6) | .139 |
| Ca2+-Blocker | 16 (38.4) | 15 (36) | .500 |
| Diuretics | 21 (50.0) | 21 (50.0) | 1.00 |
| Ambulatory BP (mm Hg, ) | |||
| SBP | 155.9 ± 23.2 | 168.6 ± 28.4 | .107 |
| DBP | 87.4 ± 12.1 | 93.9 ± 14.8 | .092 |
| Ablation points | 6.2 ± 0.8 | 11.0 ± 2.0 | .000 |
| Ablation impedance (Ω, ) | |||
| Initial | 177.9 ± 26.6 | 190.1 ± 22.4 | .115 |
| Lowest | 159.0 ± 21.9 | 167.2 ± 18.1 | .193 |
| Creatinine (mg/dL, ) | 102.1 ± 47.9 | 135.7 ± 193.5 | .455 |
| eGFR [mL/min/1.73m2, ] | 73.6 ± 24.1 | 71.8 ± 28.0 | .829 |
| Glucose (mg/Dl, ) | 6.5 ± 2.4 | 5.5 ± 2.0 | .135 |
| AST (U/L, ) | 22.2 ± 9.2 | 36.9 ± 15.1 | .339 |
| ALT (U/L, ) | 20.5 ± 14.32 | 38.6 ± 18.8 | .351 |
| Hb (g/L, ) | 133.3 ± 16.2 | 141.1 ± 26.5 | .260 |
| BNP (pg/mL, ) | 596.9 ± 220.2 | 422.3 ± 146.7 | .506 |
Notes:
- F
-
female
- M
-
male
- CAD
-
coronary artery disease
- DM
-
diabetes mellitus
- RAAS
-
renin-angiotensin-aldosterone system
- Ca 2+
-
calcium Data are given as %
- SBP
-
Systolic blood pressure
- DBP
-
Diastolic blood pressure
- AST
-
aspartate aminotransferase
- ALT
-
Alanine aminotransferase
- Hb
-
hemoglobin
- BNP
-
Brain natriuretic peptide
Results
Baseline characteristics and RDN ablation parameters
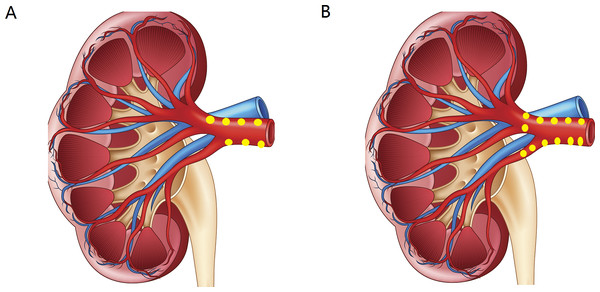
Data of 48 cases were examined, of which two cases had missing follow-up due to death, and four cases were excluded due to change in drug use, leading to 42 cases to be included for this study. The baseline characteristics of the patients included in the analysis are presented in Table 1. These 42 patients were divided into two groups according to the numbers of ablation points of RDN (Fig. 1): (1) the standard treatment group (Fig. 1A): spiral ablation from near to proximal, with less than 8 points per artery (adjacent ablation point interval 0.5 cm); ablation energy was 8–10 w, and each ablation point was ablated for 60 s (Krum et al., 2014; Symplicity HTN-2 Investigators et al., 2010; Johns, 2014; Kopp, 2011; Tsioufis et al., 2017); and (2) the intensive treatment group (Fig. 1B): from near to far by spiral ablation, with at least 8 points per artery (adjacent ablation point interval 0.25 cm); ablation energy was 8-10 w, and each ablation point was ablated for 60 s. Except for the ablation points, there was no significant difference in all of the other parameters. The average number of ablation points per patient was 9.1 ± 3.0; the average initial ablation impedance was 184.0 ± 25.1 Ω; the lowest average ablation impedance was 163.1 ± 20.3 Ω; and the range of impedance decline rate was 7.1%–14.4%, with an average of 11.1% ± 5.0%). The actual ablation temperature was between 25−46 °C and the power was between 6–13 W.
Figure 1: (A) The standard treatment group: spiral ablation from near to proximal, with less than 8 points per artery; (B) the intensive treatment group: from near to far by spiral ablation, with at least 8 points per artery.
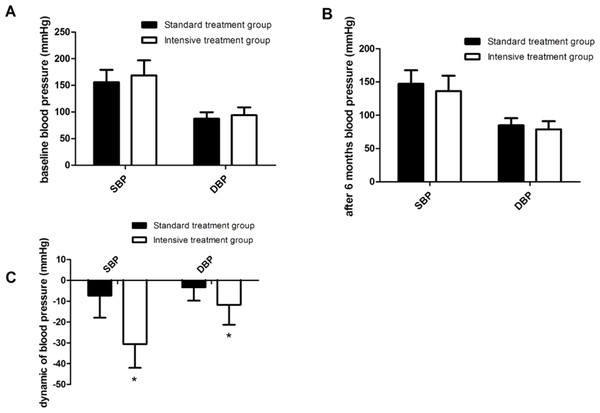
Blood pressure
Comparison of 24-hour dynamic systolic blood pressure (SBP) and diastolic blood pressure (DBP) in the standard and the intensive treatment groups showed no significant difference in baseline BP before ablation (Fig. 2A), or 6 months postoperative BP (Fig. 2B). Interestingly, the mean 24-h blood pressure decreased significantly from baseline to 6 months in the intensive treatment group (24–h systolic blood pressure decreased by 27.4 ± 11.4 mmHg, P < 0.0001; 24–h diastolic blood pressure decreased by 10.9 ± 9.6 mmHg, P = 0.005; Fig. 2C).
Figure 2: Change of systolic and diastolic 24-h AMBP 6 months after renal denervation.
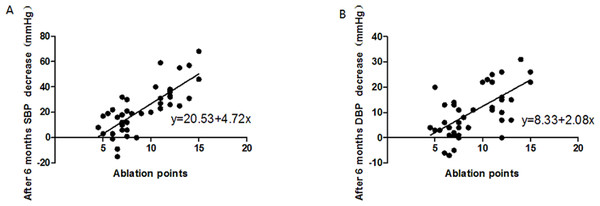
(A) shows no significant difference in baseline BP before ablation; (B) shows no significant difference in 6 months postoperative BP; (C) shows the dynamic SBP and DBP in patients received intensive treatment were significantly lower compared to patients in the standard treatment group.Correlation between the number of ablation points and mean changes of SBP and DBP after 6 months was analyzed (in mmHg; Fig. 3). The results of the mean 24-h blood pressure showed that the average SBP decline rate increased with the number of ablation points (R2 = 0.777, P < 0.01; Fig. 3A). Similar correlation pattern was also observed for DBP (R2 = 0.633, P < 0.01; Fig. 3B).
Figure 3: Correlation between the number of ablation points and mean changes of SBP and DBP after 6 months were analyzed.
(A) The results of 24-hour ABPM showed that the average SBP decline rate increased with the number of ablation points; (B) the results of 24-hour ABPM showed that the average DBP decline rate increased with the number of ablation points, but slightly lower than that of SBP.Safety index
Both treatments showed good tolerability and safety in the present study as demonstrated by the safety index parameters, with no significant difference between the two groups (Table 2). Notably, the eGFR remained unaltered 6 months after RDN in both groups. Meanwhile, none of the patients developed acute kidney injury, showed doubling of creatinine, or required dialysis.
| Baseline | 6 months after RDN | |||||
|---|---|---|---|---|---|---|
| Standard treatment | Intensive treatment | P | Standard treatment | Intensive treatment | P | |
| Creatinine (mg/dL) | 102.1 ± 47.9 | 135.7 ± 193.5 | .455 | 104.9 ± 80.8 | 170.0 ± 243.0 | .291 |
| eGFR [mL/(min/1.73m2)] | 73.6 ± 24.1 | 71.8 ± 28.0 | .829 | 82.6 ± 29.6 | 62.5 ± 28.6 | .057 |
| Glucose (mg/dL) | 6.5 ± 2.4 | 5.5 ± 2.0 | .135 | 7.8 ± 5.6 | 5.3 ± 2.3 | .115 |
| AST (U/L) | 22.2 ± 9.2 | 36.9 ± 15.1 | .339 | 18.6 ± 8.5 | 19.1 ± 7.4 | .875 |
| ALT (U/L) | 20.5 ± 14.32 | 38.6 ± 18.8 | .351 | 15.8 ± 8.6 | 15.4 ± 10.9 | .929 |
| Hb (g/L) | 133.3 ± 16.2 | 141.1 ± 26.5 | .260 | 130.2 ± 22.6 | 131.5 ± 23.8 | .883 |
| BNP (pg/mL) | 596.9 ± 220.2 | 422.3 ± 146.7 | .506 | 281.0 ± 116.7 | 184.8 ± 62.1 | .457 |
Notes:
- AST
-
aspartate aminotransferase
- ALT
-
Alanine aminotransferase
- Hb
-
hemoglobin
- BNP
-
Brain natriuretic peptide
Echocardiography
Patients of both groups were assessed for left ventricular end-diastolic diameter (LVDd), left ventricular end-systolic diameter (LVDs), interventricular septum (IVS), fractional shortening (FS), left ventricular ejection fraction (LVEF), left ventricular end-diastolic pressure (LVEDP), left ventricular systolic pressure (LVSP) and heart rate (HR) before and 6 months after RDN (Table 3). None of these values showed significant difference between the two groups at baseline before RDN. LVEF and IVS were slightly improved in the two groups, but there was no statistical difference.
| Baseline | After 6 month | |||||
|---|---|---|---|---|---|---|
| Standard treatment arm | Intensive treatment arm | P | Standard treatment arm | Intensive treatment arm | P | |
| LVEF(%) | 49.9 ± 14.9 | 50.0 ± 10.3 | .981 | 52.6 ± 14.3 | 53.9 ± 11.3 | .697 |
| LVDs(mm) | 34.9 ± 10.2 | 36.7 ± 10.2 | .535 | 36.1 ± 10.2 | 36.1 ± 8.2 | .924 |
| LVDd(mm) | 52.9 ± 7.1 | 56.1 ± 7.1 | .134 | 54.3 ± 6.7 | 55.4 ± 8.1 | .677 |
| IVS(mm) | 10.8 ± 3.1 | 12.3 ± 2.9 | .083 | 10.6 ± 2.6 | 11.3 ± 2.9 | .331 |
Notes:
- LVEF
-
left ventricular ejection fraction
- LVDd
-
Left ventricular end diastolic diameter
- LVDs
-
Left ventricular end systolic diameter
- IVS
-
interventricular septum
Adverse reactions
During the 6-month follow-up after surgery, 1 (2.4%) participant of the standard treatment experienced cardiovascular disease events or death, and 2 (4.8%) experienced other serious adverse events; while in the intensive treatment group, 3 (7.2%) participants experienced cardiovascular disease events or deaths. There was no significant difference between the two groups in the follow-up of adverse events (Table 4).
| Standard treatment | Intensive treatment | P | |
|---|---|---|---|
| Death | 1 (2.4) | 1 (2.4) | .756 |
| Stroke | 1 (0.0) | 0 (0.0) | .500 |
| Heart failure | 0 (2.4) | 2 (4.8) | .244 |
| Aneurysm | 1 (2.4) | 0 (0.0) | .500 |
Discussion
To date, researches have provided indefinite results on the antihypertensive efficacy of RDN in resistant hypertension patients, which spurred discussions on technical aspects of RDN, and further research on the role of renal nerves in the regulation of kidney function as well as the pathophysiology of hypertension. Based on this, the present study aimed to compare the antihypertensive efficacy of RDN by increasing the number of ablation points. We found that the defect of previous incomplete denervation could be made up by increasing the number of ablation points, expanding the area of ablation and increasing the depth of injury.
Although the combination of multiple drugs is more effective in controlling BP, some patients still have poor response and the incidence of cardiovascular and cerebrovascular diseases remains high. Therefore, there is an urgent need of searching for alternative ways to effectively treat hypertension, particularly resistant hypertension (Verloop, Voskuil & Doevendans, 2013; Azizi et al., 2015; deJong et al., 2016). Recent evidence indicated that hyperactivation of the renal sympathetic nerves could lead to decreased water and sodium reabsorption as well as renal blood flow and stimulate the renin-angiotensin-aldosterone system, leading to elevated BP (Henegar et al., 2015; Fengler et al., 2017; Chen et al., 2017). During the past decade, a number of studies have extensively evaluated the regulation of BP by reducing renal sympathetic activity through invasive and noninvasive treatments (Fengler et al., 2016; Mahfoud et al., 2017). Among them, percutaneous RDN is the most widely studied. The Symplicity HTN-1, HTN-2 and other large clinical studies have confirmed the effectiveness and safety of RDN in the treatment of refractory hypertension (Krum et al., 2014; Symplicity HTN-2 Investigators et al., 2010). However, the contradictory results from the Symplicity HTN-3 trial (Kandzari et al., 2012) has re-initiated a debate on the effect of RDN, as some experts believe that the ablation efficacy can be affected by various factors, such as renal artery anatomy, depth of ablation lesions and atherosclerosis, and therefore, it remains methodologically challenging to achieve complete ablation (Kandzari et al., 2015). A human autopsy study indicated that the distribution and density of renal sympathetic nerves surrounding the renal arteries was rather random (Sakakura et al., 2014). Thereafter, Fengler et al. successfully reduced norepinephrine release by co-ablating the main renal artery and its branches. The results showed that increasing the number of ablation points and altering the ablation sites had a superimposed effect (Henegar et al., 2015; Fengler et al., 2017). Consistently, recent evidence also suggested that increasing the number of radiofrequency lesions in the renal artery was effective in reducing renal sympathetic activity (Mahfoud et al., 2015). Therefore, this study adjusted the number of ablation points, expanding the ablation area, and increasing the depth of the injury.
Inconsistent findings from previous studies on the antihypertensive efficacy of renal denervation in resistant hypertension patients also inspired discussions on technical aspects of renal denervation and further research on the role of renal nerves in the regulation of kidney function as well as the pathophysiology of hypertension. The present study showed that, on the premise that the basic drugs remain unchanged, increasing the ablation points of the renal artery resulted in stronger impact of radiofrequency energy on the nerve bundle and greater reduction in BP, while causing no serious renal artery injury and adverse events. Considering the possible ablation area and the shape, depth and point of renal artery ablation, the proper helical ablation position and the degree of renal sympathetic nerve injury may have different outcomes (Kandzari et al., 2015). Tzafriri et al. (2015) also demonstrated that renal norepinephrine and BP declined significantly in response to multi-electrode therapy in animal models. BP reduction was found to be related to the size-weighted numbers of degenerative nerves, suggesting that the effectiveness of hypertension treatment depended on the extent of nerve damage and ablation (Tzafriri et al., 2015; Bertog et al., 2017). In line with these findings, our study here showed that RDN, a relatively simple and quick operation, can effectively control the BP of patients with resistant hypertension.
Limitations
Admittedly, the present study suffered from several limitations. Firstly, the number of patients enrolled in this study was relatively small, and our study may not have sufficient statistical power. The number of postoperative adverse reactions in the follow-up might be affected due to the small sample size in this study. Secondly, our study was a single-center one and all patients in this study had high BP. Therefore, the results might not be representative of the overall hypertensive population. Finally, the retrospective design was subject to selection bias.
Conclusions
The present study supported the notion that RDN could effectively control BP in patients with resistant hypertension. By comparing the different ablation points (standard versus intensive treatment) and analyzing the antihypertensive efficacy after 6 months, our results confirmed that the antihypertensive efficacy was related to the integrity of renal sympathetic activity and RDN renal ablation.