A rapid and accurate method for the detection of four aminoglycoside modifying enzyme drug resistance gene in clinical strains of Escherichia coli by a multiplex polymerase chain reaction
- Published
- Accepted
- Received
- Academic Editor
- Paul Tulkens
- Subject Areas
- Biochemistry, Biotechnology, Microbiology, Infectious Diseases, Public Health
- Keywords
- Polymerase chain reaction, Molecular detection, Multiplex polymerase chain reaction, Aminoglycoside modifying enzyme drug resistance gene
- Copyright
- © 2020 Shi et al.
- Licence
- This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, reproduction and adaptation in any medium and for any purpose provided that it is properly attributed. For attribution, the original author(s), title, publication source (PeerJ) and either DOI or URL of the article must be cited.
- Cite this article
- 2020. A rapid and accurate method for the detection of four aminoglycoside modifying enzyme drug resistance gene in clinical strains of Escherichia coli by a multiplex polymerase chain reaction. PeerJ 8:e8944 https://doi.org/10.7717/peerj.8944
Abstract
Background
Antibiotics are highly effective drugs used in the treatment of infectious diseases. Aminoglycoside antibiotics are one of the most common antibiotics in the treatment of bacterial infections. However, the development of drug resistance against those medicines is becoming a serious concern.
Aim
This study aimed to develop an efficient, rapid, accurate, and sensitive detection method that is applicable for routine clinical use.
Methods
Escherichia coli was used as a model organism to develop a rapid, accurate, and reliable multiplex polymerase chain reaction (M-PCR) for the detection of four aminoglycoside modifying enzyme (AME) resistance genes Aac(6′)-Ib, Aac(3)-II, Ant(3″)-Ia, and Aph(3′)-Ia. M-PCR was used to detect the distribution of AME resistance genes in 237 clinical strains of E. coli. The results were verified by simplex polymerase chain reaction (S-PCR).
Results
Results of M-PCR and S-PCR showed that the detection rates of Aac(6′)-Ib, Aac(3)-II, Ant(3″)-Ia, and Aph(3′)-Ia were 32.7%, 59.2%, 23.5%, and 16.8%, respectively, in 237 clinical strains of E. coli. Compared with the traditional methods for detection and identification, the rapid and accurate M-PCR detection method was established to detect AME drug resistance genes. This technique can be used for the clinical detection as well as the surveillance and monitoring of the spread of those specific antibiotic resistance genes.
Introduction
With the abuse and misuse of antibiotics, bacterial tolerance is becoming an increasingly serious concern (Ferri et al., 2017; Levin-Reisman et al., 2017), leading to the emergence of a series of drug-resistant bacteria (multi-drug-resistance (MDR), extensively-drug-resistant (XDR), and pan-drug-resistant (PDR)) (Healey et al., 2016; Planet, 2017). MDR is defined as acquired non-susceptibility to at least one agent in three or more antimicrobial categories. XDR is defined as non-susceptibility to at least one agent in all but two or fewer antimicrobial categories. PDR is defined as non-susceptibility to all agents in all antimicrobial categories (Magiorakos et al., 2012). Aminoglycoside antibiotics (Amikacin, Gentamicin, Tobramycin, Kanamycin, Netilmicin, Streptomycin, and Neomycin) (Doi, Wachino & Arakawa, 2016; Krause et al., 2016; Yadegar et al., 2009) are mainly used to treat infections caused by aerobic Gram-negative bacteria, such as Escherichia coli and Klebsiella pneumoniae, and non-fermenters like Pseudomonas aeruginosa (Jana & Deb, 2006; Magnet & Blanchard, 2005; Zavascki, Klee & Bulitta, 2017). However, bacteria can easily develop tolerance to aminoglycoside antibiotics due to the production of aminoglycoside modifying enzymes (AMEs) (Haidar et al., 2016; Khosravi, Jenabi & Montazeri, 2017) and the rapid transmission of AME resistance genes in pathogenic bacteria (Ramirez & Tolmasky, 2010). The severity of antibiotic tolerance has become a global worldwide concern. The theme of World Health Day in 2011 was “Combat Drug Resistance: No action today, No cure tomorrow” (Chellat, Raguz & Riedl, 2016; Tseng et al., 2012), whereas that in 2018 was “Change Can’t Wait. Our Time with Antibiotics is Running Out”. In such a severe situation of drug resistance, there is an urgent need to identify the species of bacteria and their drug resistance genes accurately and quickly to guide clinical drug use (Brossier et al., 2017; Mu et al., 2016). This need led to the establishment of a rapid, accurate, and economical method to detect pathogens and their drug resistance as early as possible. Such a technique is helpful for the rational use of drugs in clinical practice, as well as of great clinical significance to control and shorten the course of the disease (Laamiri et al., 2016).
Although the traditional method for bacterial resistance identification is simple and economical, identification is completed in about 4–7 days (Jami Al-Ahmadi & Zahmatkesh Roodsari, 2016; Phaneuf et al., 2013). It includes several steps, such as bacterial culture, single colony isolation, colony morphology observation, biochemical identification, and serotype identification (Panek, Frac & Bilinska-Wielgus, 2016). The accuracy of this method is low, and errors easily occur (Tuttle et al., 2011). The main methods used to test drug sensitivity include the disk diffusion method, E-test, dilution method (agar and broth dilution method), and automatic instruments (Biswas, 2016; Ghosh et al., 2015). Such methods have the advantages of low cost, easy operation, and strong flexibility. However, they also feature some inevitable disadvantages, such as slow, empirical dependance. With the development of biological science and technology, many new biological technologies have entered people’s lives. Interspecific and intraspecific conserved nucleic acid sequences have been discovered in succession (Nagar & Hahsler, 2013), and various bioinformatics and molecular biological techniques based on nucleic acid amplification have been used to identify pathogens; an example of such techniques is polymerase chain reaction (PCR), which has become the gold standard (Tuttle et al., 2011).
Multiplex polymerase chain reaction (M-PCR) (Chamberlain et al., 1988) usually means that two or more pairs of primers exist in one PCR reaction system at the same time; it can amplify multiple target bands at one time (Henegariu et al., 1997). Its reaction principle, operation steps, and general composition of the required reagents are basically the same as those of simplex PCR (S-PCR). To date, M-PCR has been widely used in many fields, such as scientific research and disease diagnosis, especially in the simultaneous detection of pathogenic microorganisms, hereditary diseases, and oncogenes (Azizi et al., 2016; Skodvin et al., 2017). What’s more, M-PCR can also be used in the simultaneous detection of multidrug resistance genes in pathogenic bacteria (Hong et al., 2009). Compared with traditional drug sensitivity test and S-PCR, M-PCR is fast, efficient, and able to timely guide the clinical antibiotic therapy (Chavada & Maley, 2015; Lee et al., 2014; Park & Ricke, 2015). M-PCR has higher efficiency than S-PCR, and the former can detect a variety of pathogenic bacteria or drug-resistant genes simultaneously in one reaction system (Kim, Hwang & Kim, 2017). At the same time, M-PCR can reduce any experimental errors that may occurs during the experiment.
Among the AME resistance genes, Aac(6′)-Ib, Aac(3)-II, Ant(3″)-Ia, and Aph(3′)-Ia are the most widely distributed (Costello et al., 2019; Haldorsen et al., 2014; Nasiri et al., 2018; Odumosu, Adeniyi & Chandra, 2015; Ojdana et al., 2018; Vaziri et al., 2011; Xiao & Hu, 2012). Given that the M-PCR can detect multiple genes simultaneously, we aimed to develop a M-PCR system for the detection of the four most widely spread AME genes. The reaction system was verified in 237 clinical E. coli strains.
Materials and Methods
Bacterial strains and culture
The 237 clinical strains of E. coli used in this study were provided, isolated, cultured, and identified by the First People’s Hospital of Yunnan Province. All the strains were cultured in Luria-Bertani (LB) liquid medium in a shaking incubator at 37 °C and 180 rpm for 12 h. The bacterial genome was extracted using the TIANamp genomic DNA kit following the manufacturer’s protocol and then stored at −40 °C for further experiments.
Search of drug resistance genes searching and design of primers
Four AME resistance genes Aac(6′)-Ib, Ant(3″)-Ia, Aph(3′)-Ia, and Aac(3)-II were downloaded from the Comprehensive Antibiotic Resistance Database (https://card.mcmaster.ca/). The primers were designed according to the conservative region and synthesized by TSINGKE Biological Technology. The primers sequences are shown in Table 1.
| Gene | Primers | Sequence (5′–3′) | Product size (bp) | Annealing temperature (°C) |
|---|---|---|---|---|
| Aac(6′)-Ib | Aac(6′)-I-F | AAACCCCGCTTTCTCGTAGC | 112 | 57 |
| Aac(6′)-I-R | AAACCCCGCTTTCTCGTAGC | |||
| Ant(3″)-Ia | Ant(3″)-F | CCGGTTCCTGAACAGGATC | 180 | 59 |
| Ant(3″)-R | CCCAGTCGGCAGCGACATC | |||
| Aph(3′)-Ia | Aph(3′)-F | CAAGATGGATTGCACGCAGG | 317 | 56 |
| Aph(3′)-R | TTCAGTGACAACGTCGAGCA | |||
| Aac(3)-II | Aac(3)-II-F | GCTCGGTTGGATGACAAAGC | 379 | 57 |
| Aac(3)-II-R | AGGCGACTTCACCGTTTCTT |
Establishment of S-PCR reaction system
S-PCR was performed using 2X Tsingke Master Mix, which was purchased from Tsingke Biotech Co., Ltd. (Kunming, China). According to the manufacturer’s protocol, the S-PCR reaction system containing 12.5 µL of 2X Tsingke Master Mix, 1 µL of primers (10 µM), and 1 µg of DNA template from each strain was added with nuclease-free water up to 25 µL. The reactions were performed in a GeneAmp PCR System 9700 (Thermo Fisher Scientific, Inc., Waltham, MA, USA) with the following amplification conditions: pre-denaturation at 95 °C for 5 min; 30 cycles of denaturation at 95 °C for 30 s, annealing at 57 °C, 59 °C, 56 °C, and 57 °C (Aac(6′)-Ib, Ant(3″)-Ia, Aph(3′)-Ia, and Aac(3)-II) for 30 s; extension at 72 °C for 30 s; and a final extension at 72 °C for 7 min. The S-PCR products were verified using gel electrophoresis on a 2% agarose gel and stained with GelStain (Beijing Transgen Biotech Co., Ltd., Beijing, China).
Construction and verification of positive plasmids
The positive plasmids with resistance genes were constructed as described in a previous study (Li et al., 2019). In brief, the DNA fragments of the target genes were obtained by PCR reactions using the genomic DNA of E. coli as a template. The target fragment was inserted into the pMD 19-T simple vector and transformed into JM109-competent cells. The positive clones were selected for overnight culture to extract plasmids. Finally, the copies of recombinant plasmids were calculated.
Sensitivity and accuracy evaluation of S-PCR
After the positive plasmids were constructed, the sensitivity of S-PCR reactions was evaluated using the serially diluted 10-fold positive plasmids. According to the resistance gene information of 237 clinical strains of E. coli provided by the First People’s Hospital of Yunnan Province, the strains with Aac(6′)-Ib, Ant(3″)-Ia, Aph(3′)-Ia, and Aac(3)-II resistance genes were screened to evaluate accuracy.
Establishment of M-PCR reaction system and accuracy evaluation of M-PCR
The M-PCR was performed by using a Multiplex PCR kit (Nanjing Vazyme Biotechnology Co., Ltd., Nanjing, China). According to the manufacturer’s protocol, the M-PCR reaction system containing 25 µL of 2X Multiplex Buffer, 10 µL of 5X Multiplex GC Enhancer, 1 µL of each primer (10 µM), 1 µL of Multiplex DNA polymerase, and 1 µg of DNA template from each strain, was added with nuclease-free water up to 50 µL. The reactions were performed in a GeneAmp PCR System 9700 (Thermo Fisher Scientific, Inc., Waltham, MA, USA) with the following amplification conditions: pre-denaturation at 95 °C for 5 min, followed by 30 cycles of denaturation at 95 °C for 30 s, annealing at 60 °C for 3 min, extension at 72 °C for 3 min, and a final extension at 72 °C for 30 min. The M-PCR products were verified by gel electrophoresis on 2% agarose gel and stained with GelStain (Beijing Transgen Biotech Co., Ltd., Beijing, China).
Based on the drug sensitivity information of 237 clinical strains of E. coli, five isolates (1611NY0004, 1611UR0282, 1611SP0549, 1611UR0062, and 1611UR0215) previously tested for the Aac(6′)-Ib, Ant(3″)-Ia, Aph(3′)-Ia, and Aac(3)-II by S-PCR were tested for the M-PCR.
Sensitivity evaluation of M-PCR
The sensitivity of M-PCR was performed by using gradient dilution plasmids and bacterial solution. The four equal concentration plasmids with Aac(6′)-Ib, Ant(3″)-Ia, Aph(3′)-Ia, and Aac(3)-II resistance genes were mixed together and serially diluted to 10-fold (108–100). E. coli 1611NY0004 was selected as the representive strain for sensitivity evaluation. The stain was cultured in LB liquid medium to OD600 = 1, and the colony-forming units of bacterial solution were calculated by the plate count method. The bacterial solution was serially diluted as 10-fold (108–100).
M-PCR detection for clinical samples
All the 237 clinical E. coli strains were provided and identified by the First People’s Hospital of Yunnan Province and used in the accuracy evaluation of S-PCR and M-PCR.
Results
Establishment of S-PCR reaction system
The positive plasmids with drug resistance genes (Aac(6′)-Ib, Ant(3″)-Ia, Aph(3′)-Ia, and Aac(3)-II) were successfully constructed, with 3 × 109, 4 × 109, 5 × 109 and 4 × 1010 copies/μL (114.5, 141.2, 156.8 and 153.2 ng/μL), respectively. The S-PCR reaction template comprised the serially diluted plasmids. Meanwhile, the four drug resistance genes were detected in the 237 clinical strains of E. coli, and the bacterial solution was the S-PCR template. As shown in Fig. 1, the limitation for the detection of the four drug resistance genes was 100 copies/μL. The accuracy rate for the detection of drug resistance genes was 100% (partially representative results), which was consistent with the hospital data (Table S1).
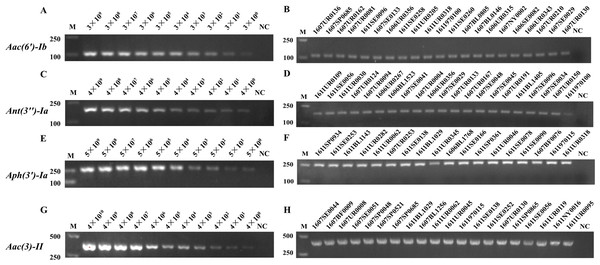
Figure 1: The sensitivity and accuracy evaluation of Aac(6′)-Ib, Ant(3″)-Ia, Aph(3′)-Ia, and Aac(3)-II resistance genes by S-PCR.
The serially diluted positive plasmids with resistance gene were used as the template in the sensitivity evaluation of S-PCR. (A) Aac(6′)-Ib, 3 × 109−3 × 100 copies/µL. (C) Ant(3″)-Ia, 4 × 109−4 × 100 copies/µL. (E) Aph(3′)-Ia, 5 × 109−5 × 100 copies/µL. (G) Aac(3)-II, 4 × 1010−4 × 100 copies/µL. Meanwhile, the four resistance genes were detected in the 237 clinical strains of E. coli respectively, the bacterial solution as the S-PCR template. (B) The accuracy evaluation of Aac(6′)-Ib resistance genes. (D) The accuracy evaluation of Ant(3″)-Ia resistance genes. (F) The accuracy evaluation of Aph(3′)-Ia resistance genes. (H) The accuracy evaluation of Aac(3)-II resistance genes. All experiments were repeated six times. The nuclease-free water used as template for NC (Negative control). M, marker.Establishment of M-PCR reaction system
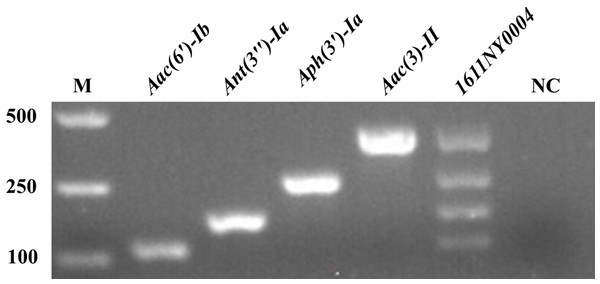
After the S-PCR reaction system was established and optimized (data not shown), the M-PCR reaction system was constructed. As shown in Fig. 2, Aac(6′)-Ib, Ant(3″)-Ia, Aph(3′)-Ia, and Aac(3)-II with 112, 180, 317, and 379 bp, respectively, were amplified successfully. E. coli 1611NY0004 with the four drug resistance genes was used as the positive control template for the M-PCR reaction. In the M-PCR reaction system, the four drug resistance genes could be amplified well simultaneously.
Figure 2: Establishment of M-PCR reaction system.
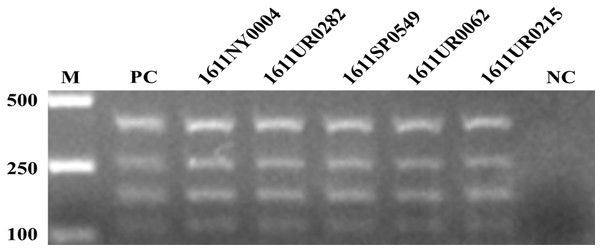
Accuracy evaluation of M-PCR
The five clinical E. coli strains (1611NY0004, 1611UR0282, 1611SP0549, 1611UR0062, and 1611UR0215) with four resistance genes were screened for the accuracy evaluation of M-PCR. The four equal concentration plasmids with Aac(6′)-Ib, Ant(3″)-Ia, Aph(3′)-Ia, and Aac(3)-II resistance genes were mixed together as the positive control. As shown in Fig. 3, the four resistance genes were successfully amplified by M-PCR in the tested strains, which was consistent with the resistance gene information provided by the hospital.
Figure 3: The accuracy evaluation of M-PCR.
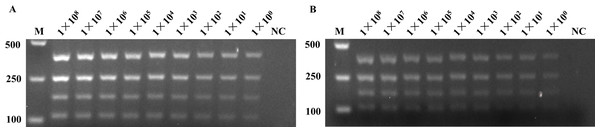
Sensitivity evaluation of M-PCR
The gradient dilution of plasmids and bacterial solution was used in the sensitivity evaluation of M-PCR. The gradient dilution of plasmids was the mixture of the four equal concentration plasmids with Aac(6′)-Ib, Ant(3″)-Ia, Aph(3′)-Ia, and Aac(3)-II resistance gene and then serially diluted as 10-fold (108–100 copies/mL). The E. coli 1611NY0004 strain was used in the gradient 10-fold (108–100 CFU/mL) dilution of bacterial solution for sensitivity evaluation. As shown in Fig. 4, the detection system could reach the detection limit of 100 copies/mL or 100 CFU/mL at the plasmid level and bacterial liquid level.
Figure 4: The sensitivity evaluation of M-PCR.
The gradient dilution of plasmids and bacterial solution was used in the sensitivity evaluation of M-PCR. (A) The four equal concentration plasmids with Aac(6′)-Ib, Ant(3″)-Ia, Aph(3′)-Ia, and Aac(3)-II resistance genes were mixed, and serially diluted as 10-fold (1 × 108−1 × 100), as the sensitivity evaluation of M-PCR. The nuclease-free water used in lane 10 as template for NC. (B) The E. coli 1611NY0004 strain with four resistance genes was used as the template for the the sensitivity evaluation of M-PCR. The bacterial solution was serially diluted as 10-fold (1 × 108−1 × 100). The nuclease-free water used in lane 10 as template for NC. NC, negative control; M, marker.Detection of clinical samples by multiplex PCR
All the 237 E. coli strains were detected by S-PCR and M-PCR. The detection results and the accuracy are shown in Table S1. The results showed that the detection rates of Aac(6′)-Ib, Aac(3)-II, Ant(3″)-Ia, and Aph(3′)-Ia were 32.7%, 59.2%, 23.5% and 16.8% in 237 clinical strains of E. coli, respectively. These values were consistent with the gene information of the strains given by the hospital.
Discussion
Antibiotics are considered the most effective drugs in the treatment of infectious diseases (Elder, Kuentz & Holm, 2016). The emergence of antibiotics changed the outcome of infectious diseases and extended life expectancy (Wagner & Maynard, 2018). However, given the overuse and misuse of antibiotics, MDR strains have emerged (Elder, Kuentz & Holm, 2016). Therefore, rapid and accurate methods for the detection of bacterial resistance are urgently needed, and the use of antibiotics or antibiotic therapy should be more standardized and technically, where possible, monitored. With the development of molecular biology and bioinformatics, the detection methods of bacterial drug resistance genes, including PCR, loop-mediated isothermal amplification, and whole genome sequencing (WGS) (Moran et al., 2017; Su, Satola & Read, 2019), have increased (Tamburro & Ripabelli, 2017). Although WGS is gradually reaching maturity, while sequencing costs are drastically decreasing, it is however still relatively costly, complex in operation and requires for analysis specialized personnel like bioinformaticians, which limits its popularization and application (Quainoo et al., 2017). M-PCR is widely used in the identification and drug resistance detection of bacteria for its rapid, sensitive, economy-friendly and high-effect characteristics (Pham et al., 2017).
Aminoglycoside antibiotics are one of the most widely used antibiotics, and the main reason for aminoglycoside antibiotic resistance is the production of AME. Aminoglycoside antibiotic resistance is related to the AME drug resistance genes Aac(6′)-Ib, Aac(3)-II, Ant(3″)-Ia, and Aph(3′)-Ia (Zarate et al., 2018). Thus, this study designed primers for the four drug resistance genes and constructed a four-drug resistance genes detection system, which greatly improved the detection efficiency and shortened the detection time.
The MDR gene detection system was established successfully in this experiment, and it exhibited the advantages of high efficiency, rapidity, and high performance-to-price ratio compared with the S-PCR reaction system. The MDR gene detection system also fully met the requirements for the clinical detection of pathogens and drug resistance. In this experiment, the four drug-resistant genes were identified in the five representative E. coli MDR bacteria by M-PCR. The results obtained by M-PCR were consistent with those of S-PCR, thereby indicating the accuracy of M-PCR. The M-PCR detection system was applied to the detection of 237 clinical strains of E. coli. On the basis of the drug resistance gene information given by the hospital, the accuracy rate of M-PCR could reach 100%; the detection rates of Aac(6′)-Ib, Aac(3)-II, Ant(3″)-Ia, and Aph(3′)-Ia were 32.7%, 59.2%, 23.5% and 16.8%, respectively. These findings indicated the potential of reintroducing additional resistant genes into the M-PCR system to detect numerous genes at a time. Even the specific genes of the bacteria could be added into the M-PCR system for the identification of bacterial species. From the detection rate of the four aminoglycoside modifying enzyme resistance genes, Aac(3)-II had the highest detection rate in the 237 clinical strains of E. coli. This result suggested that the resistance of three aminoglycoside antibiotics gentamicin, tobramycin, and netilmicin resistance is widespread in bacterial infections and should be avoided.
Conclusion
The M-PCR system developed in this study could amplify the four genes with very extremely high sensitivity to 100 copies. The sensitivity rate of M-PCR was higher than that of most previously reported studies, which proved the sensitivity of this technique. Moreover, the M-PCR detection method greatly reduced the detection time and improved the detection efficiency. M-PCR in this study demonstrated high sensitivity and efficiency, low price, and other characteristics but not one-to-one correspondence between genotype and phenotype. Therefore, simply detecting genes failed to completely determine the phenotype, but the four genes selected genes had the highest prevalence of aminoglycoside antibiotic resistance. We conducted the simultaneous detection of these four genes to compensate for the limitations of detecting one gene, thereby making our methodology reliable and persuasive. Our method was established to assist medical institutions to predict drug resistance, to provide an accurate direction for clinical drug selection, and to meet the needs of both doctors and patients for rapid diagnosis. In the future, we will propose a rapid drug sensitivity identification technique based on phenotype. We will also combine traditional detection methods with modern molecular techniques, starting from the phenotype, for the accurate identification of bacterial drug resistance.
Supplemental Information
Resistance genes information and the detection results of S-PCR, M-PCR of 237 clinical Escherichia coli.
Note: SPEC_NUM and SPEC_TYPE means the specimen number and type. AMK_NM, GEN_NM, and TOB_NM means the resistance of amikacin, gentamicin, and tobramycin antibiotics. SP, UR, SE, BF,DG, BL, SW, ST means the sputum, clearing urine, secretion, excreta, blood, surgical incision, and stool of the patients, respectively.