Postoperative hyperlactatemia and serum lactate level trends among heart transplant recipients
- Published
- Accepted
- Received
- Academic Editor
- Vladimir Uversky
- Subject Areas
- Biochemistry, Anesthesiology and Pain Management, Cardiology, Hematology, Surgery and Surgical Specialties
- Keywords
- Heart transplantation, Postoperative management, Intensive Care Unit, Serum lactate level, Lactic acidosis, HTX, Early recipient care, Transplantology
- Copyright
- © 2020 Kędziora et al.
- Licence
- This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, reproduction and adaptation in any medium and for any purpose provided that it is properly attributed. For attribution, the original author(s), title, publication source (PeerJ) and either DOI or URL of the article must be cited.
- Cite this article
- 2020. Postoperative hyperlactatemia and serum lactate level trends among heart transplant recipients. PeerJ 8:e8334 https://doi.org/10.7717/peerj.8334
Abstract
Background
Advanced heart failure (HF), that affects 10% of the HF population, is associated with high mortality rate, meeting 50% at 1-year from diagnosis. For these individuals, heart transplantation (HTX) remains the ultimate and the gold-standard treatment option. Serum lactate level measurements has been proven useful for determining the outcome following other cardiac surgeries and among critically ill patients. Increased serum lactate levels are expected following HTX; however, no detailed analysis has been yet performed in this population. The research aims to estimate the prevalence of hyperlactatemia and describe early postoperative serum lactate level trends among heart transplant recipients.
Materials and Methods
Forty-six consecutive patients, who underwent HTX between 2010 and 2015, were enrolled into the retrospective analysis. Serum lactate level measurements within first 48 hours post-HTX were obtained every 6 hours from routinely conducted arterial blood gas analyses. The threshold for hyperlactatemia was considered at >1.6 mmol/L, according to upper limit of normal, based on internal laboratory standardization. The highest observed measurement within the observation, regardless of the time point of observation was determined for each patient individually and was appointed as Peak Value.
Results
Consecutively measured serum lactate levels differed in time (p = 0.000), with the initial increase and subsequent decrease of the values (4.3 vs. 1.9 mmol/l; p = 0.000). The increase from the baseline level to the Peak Value was statistically significant (4.3 vs. 7.0 mmol/l; p = 0.000). Various serum lactate level trends were identified, with one or more hyperlactatemia episodes. Eventually, 50% of the individuals had normal serum lactate levels at the end of the study, and hyperlactatemia was observed in the other half.
Conclusions
Throughout the observation, all of the patients experienced at least one episode of hyperlactatemia, with the median Peak Value of 7.0 (4.5–8.4) mmol/L. Various serum lactate level trends can be identified in post-HTX patients. Further research is required to determine the clinical usefulness of newly reported serum lactate level trends among heart transplant recipients.
Introduction
Heart failure (HF), with the current prevalence of 2.5%, is a major public health problem associated with significant hospital admission rates, mortality, and health care costs (Benjamin et al., 2017). The age-adjusted rate for heart failure-related deaths has been steadily increasing since 2012, reaching 84.0 deaths per 100,000 standard population in 2014 (Ni & Xu, 2015). Advanced HF, that affects 10% of the HF patients, is associated with even higher mortality rate, meeting 50% at 1-year from diagnosis (Lund, 2018). For these individuals, heart transplantation (HTX) remains the ultimate and the gold-standard treatment option (Ponikowski et al., 2016). Nevertheless, despite the total of approximately 5,000 HTX performed worldwide annually (Khush et al., 2018), there is still a gap in scientific evidence in terms of early postoperative management for heart transplant recipients. The immunosuppression, anti-infective prophylaxis, and pulmonary hypertension treatment have been widely discussed in this group of patients (Costanzo et al., 2010), however, only few postoperative biochemical measurements have been thoroughly analyzed so far (Wierzbicki et al., 2014; Madershahian et al., 2008).
Under basal conditions, the lactate is produced by all tissues and reutilized at a nearly constant rate by the liver. Normally, lactate concentration in the extracellular fluid is about one mmol/l. The diagnostic lower and upper limits of normal slightly vary (from 0.3 to 2.0 mmol/l) according to the specimen (arterial or venous blood) and method used (Toffaletti, 1991). The overproduction and, therefore, increased levels can be observed during tissue oxygen deficiency as a result of the circulatory shock and perfusion failure (Adeva-Andany et al., 2014). The potential usefulness of lactate measurements as an indicator of the shock severity has been has been first evaluated in 1964 (Broder & Weil, 1964). Since then, numerous studies have reported data for measurements taken in various acute clinical settings and, throughout time, cut-off values for therapeutic management have evolved (Zhou et al., 2017).
Similarly, hyperlactatemia assessment has been proven useful in determining the outcome in some cardiosurgical procedures, as it reflects the problem of postoperative hypoperfusion (Hajjar et al., 2013; Andersen et al., 2015; Lopez-Delgado et al., 2015). Following HTX, increased serum lactate levels are expected, as prolonged cardiopulmonary bypass (CPB) time and compromised hemodynamic function within early postoperative hours are commonly observed. However, postoperative serum lactate level trends and clinical usefulness of lactate measurements have never been analyzed before among post-HTX patients. Moreover, currently available guidelines for the care of heart transplant recipients are mostly based on the consensus of opinion of the experts (level of evidence C) (Costanzo et al., 2010), which indicates the gap in scientific evidence.
Therefore, the presented research aims to estimate the actual prevalence of hyperlactatemia and describe early postoperative serum lactate level trends among heart transplant recipients.
Material and Methods
Forty-six consecutive patients, who underwent HTX in the Department of Cardiovascular Surgery and Transplantology between 2010 and 2015, were enrolled into the retrospective analysis. Serum lactate level measurements within first 48 h post-HTX were obtained from arterial blood gas (ABG) analyses, that were routinely conducted every 6 h. The mean age of the study group was 48.7 ± 11.7 years. The majority of the patients were males (89.1%) and were qualified for HTX due to dilated cardiomyopathy (73.9%) (Table 1).
| Variable | Analyzed population; n = 46 |
|---|---|
| Age, years | 48.7 ± 11.7 |
| Male sex, n(%) | 41 (89.1) |
| Dilated cardiomyopathy, n(%) | 34 (73.9) |
| Ischemic cardiomyopathy, n(%) | 12 (26.1) |
| Dyslipidemia, n(%) | 16 (34.8) |
| Hypertension, n(%) | 21 (45.7) |
| Diabetes, n(%) | 12 (26.1) |
Consecutive serum lactate level measurements, that were taken every 6 h, were appointed as Lac, with the following number as the time point (hour) of observation. The baseline measurement was defined as the observation taken at Intensive Care Unit (ICU) admission (Lac 0). The end of the study measurement was defined as the observation taken at the 48th hour post-HTX (Lac 48). The highest observed measurement within the observation, regardless of the time point of observation was determined for each patient individually and was presented as the Peak Value. The threshold for hyperlactatemia (>1.6 mmol/L) was defined by the upper limit value of the normal range for serum lactate concentration (0.5–1.6 mmol/l), based on internal laboratory standardization for ABG analysis. ABG analysis was performed with an automated electrode analyzer (Arterial Blood Gases-Clinical Methods-NCBI Bookshelf, 0000).
The study obtained the Jagiellonian University Bioethics Committee approval (122.6120.74.2017). According to the approval, verbal consent was obtained from all living patients.
Statistical analysis
Statistical analysis was performed with IBM® SPSS® Statistics 25. Normal distribution was tested using the Shapiro–Wilk test. Continuous variables are presented as means and standard deviation (±SD) or medians and interquartile ranges (IQR). For categorical variables, numbers and proportions are reported. Non-parametric tests for independent (Kruskal–Wallis test) or dependent samples (Wilcoxon signed-rank test, Friedman test), where appropriate, were calculated to determine the differences between observations.
Results
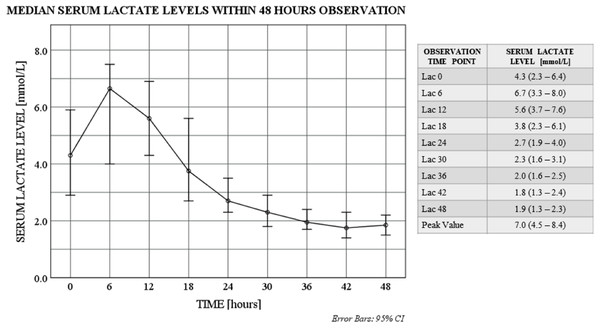
The values of the consecutive serum lactate level measurements differed in time (p = 0.000; Friedman test) and initial increase with subsequent decrease throughout the study was observed. The increase from the baseline level (Lac 0) to the highest observed value (Peak Value) was statistically significant (p = 0.000; Wilcoxon signed-rank test), and similarly was the decrease throughout the observation (from Lac 0 to Lac 48; p = 0.000; Wilcoxon signed-rank test) (Fig. 1).
Figure 1: Serum lactate level trends within 48 hours observation.
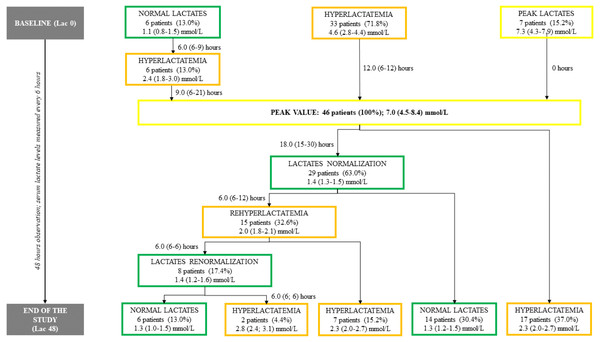
Serum lactate level distributions differ in time: χ2(2) = 169.1; p = 0.000; Friedman test. Serum lactate level medians differ between baseline (Lac 0) and end of the study (Lac 48): p = 0.000; Wilcoxon signed-rank test. Serum lactate level medians differ between baseline (Lac 0) and peak time point (Peak Value): p = 0.000; Wilcoxon signed-rank test Data for serum lactate levels are presented as medians (IQR). Lac X—consecutive serum lactate measurements with the following number as the time point (hour) of observation. Peak Value—the highest observed serum lactate level within the observation, regardless of the time point.In the detailed analysis, various serum lactate level trends were identified. In the majority of the patients (63%) serum lactate level normalization was achieved, however, one-third (33%) of the study group experienced sequent episode of hyperlactatemia after first normalization. Eventually, 50% of the individuals had normal serum lactate levels at the end of the study (Lac 48), and hyperlactatemia was observed in the other half (Fig. 2).
Figure 2: Study flow chart.
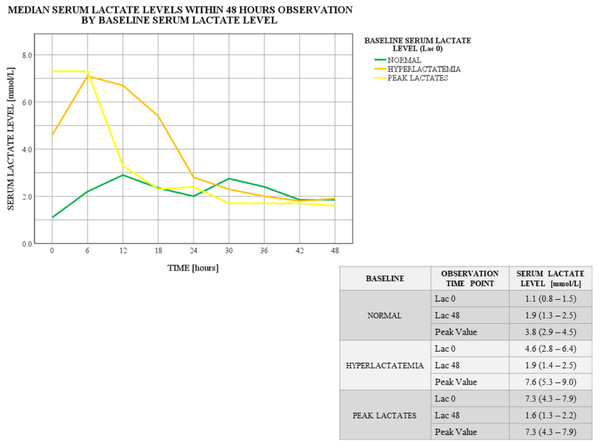
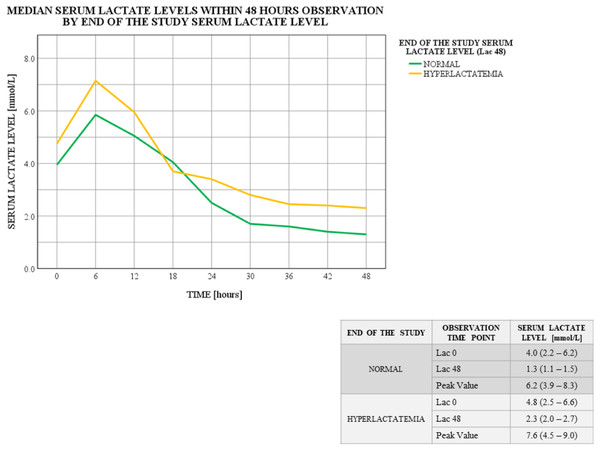
Data for time intervals and serum lactate levels are presented as medians (IQR). The number of patients at each point is followed by the % based on the total number of patients in the study. Lac X –consecutive serum lactate measurements with the following number as the time point (hour) of observation. Peak Value—the highest observed serum lactate level within the observation, regardless of the time point.Further calculations determined the association between the baseline serum lactate level (Lac 0 as normal or hyperlactatemia or peak lactates) and the highest observed serum lactate level (Peak Value) (p = 0.06; Kruskal–Wallis test; Fig. 3). No such association was found for the end of the study serum lactate level (Lac 48 as normal or hyperlactatemia) (p = 0.263; Kruskal–Wallis test; Fig. 4).
Figure 3: Serum lactate level trends within 48 hours observation by baseline serum lactate level.
Baseline (Lac 0) serum lactate level distributions differ among the groups: p = 0.000; Kruskal–Wallis test. Peak (Peak Value) serum lactate level distributions differ among the groups: p = 0.06; Kruskal–Wallis test. Data for serum lactate levels are presented as medians (IQR). Lac X—consecutive serum lactate measurements with the following number as the time point (hour) of observation. Peak Value—the highest observed serum lactate level within the observation, regardless of the time point.Figure 4: Serum lactate level trends within 48 hours observation by end of the study serum lactate level.
End of the study (Lac 48) serum lactate level distributions differ among the groups: p = 0.000; Kruskal–Wallis test. Data for serum lactate levels are presented as medians (IQR). Lac X –consecutive serum lactate measurements with the following number as the time point (hour) of observation. Peak Value—the highest observed serum lactate level within the observation, regardless of the time point.Discussion
Under anaerobic conditions, cellular metabolism converts pyruvate to lactate. Therefore, serum lactate levels relate to the oxygen debt and correspond with the severity of tissue hypoperfusion (Adeva-Andany et al., 2014; Hoshino, Kinoshita & Ono, 2018). The normal plasma lactate concentration for ABG is reported from 0.3 to 1.6 mmol/L (Broder & Weil, 1964), whereas lactic acidosis is generally defined with a threshold of greater than four mmol/L, even in the absence of overt acidemia. Type A lactic acidosis, that is considered to be a medical emergency and is associated with poor prognosis when left untreated, is usually caused by significant tissue hypoperfusion (Andersen et al., 2013).
Hyperlactatemia is a common phenomenon following cardiac surgeries, as it can result from not only hypoxic but also nonhypoxic causes such as drug therapy, cardioplegia, hypothermia, and CPB. Previous studies among cardiosurgical patients, comparing survivors vs. non-survivors, have indicated that that higher lactate levels upon ICU admission (2–3 mmol/l), or within early postoperative hours (3–4 mmol/l), are associated with increased perioperative risk and prolonged hospital stay (Hajjar et al., 2013; Lopez-Delgado et al., 2015; Andersen et al., 2015).
Nevertheless, to date only two studies, concerning the issue of postoperative hyperlactatemia among heart transplant recipients have been published. Both of the researches were single center studies that evaluated solely whether the patient has reached the threshold, set by the authors, at any time point throughout the observation. The extreme hyperlactatemia was defined by Hsu et al. as the serum lactate level greater than 15 mmol/L and occurred in 3 patients at the ICU admission and in 9 others within early postoperative hours (12/58 patients). In spite of the further serum lactate level decrease below four mmol/L, one-third of the analyzed hyperlactatemia subgroup deceased within the hospitalization, and the others within nearly 5 years post-HTX (Hsu et al., 2015). In another study, the cut-off level of four mmol/L was set according to the guidelines for severe sepsis and septic shock treatment. Based on this estimation, elevated serum lactate levels were observed among 59.2% of post-HTX patients, with higher occurrence of postoperative pulmonary complications within this subgroup. As no in-hospital deaths were reported, no testing was performed to determine the impact on early mortality (Hoshino, Kinoshita & Ono, 2018). Nevertheless, the detailed exploration of the cut-off value, appointed by the upper limit of normal for serum lactate concentration, has never been presented in post-HTX patients before.
In the presented research, hyperlactatemia was considered with the of >1.6 mmol/l, same as it is for other cardiac surgeries and non-surgical patients in our center. Despite the initially emerging pattern with early peak of the lactate values, that was similar to other post-HTX lactate analyses (Hsu et al., 2015; Hoshino, Kinoshita & Ono, 2018), more detailed evaluation revealed various serum lactate level trends. The interpretation of the initial results indicates the increase to the highest serum lactate level within first 6 postoperative hours with subsequent gradual decrease (Fig. 1). However, close case-by-case investigation provided more rigorous outcome, showing differences in the number of hyperlactatemia episodes and time intervals in between (Fig. 2).
Serum lactate level trends significantly differed between subgroups assigned based on the baseline serum lactate level (Lac 0 as normal or hyperlactatemia or peak lactates). The highest observed measurement (Peak Value) varied between the subgroups. Although the lowest Peak Value was seen in the normal group, two serum lactate level spikes can be identified (12th and 30th hour of observation). Based on the metadata, in half of these patients Peak Value was noted at 12th hour post-surgery, and in the other half later within observation. Moreover, one-third of these individuals actually experienced sequent hyperlactatemia episode (Fig. 3). On the other hand, patients who entered the study with their highest serum lactate levels (Lac 0 as peak lactates), completed the analysis with lowest values after a considerable curve slope within first 12 h of observation (Fig. 3). Similar curve slope difference was noted among the subgroups assigned by the 48th hour measurement (Lac 48 as normal or hyperlactatemia), however, this trend changed at 18th hour of observation, resulting in elevated serum lactate levels at the end of the study in the hyperlactatemia subgroup (Fig. 4).
The planned extension of this study includes the search for pre- and intraoperative factors determining various serum lactate level trends, as well as for the association between various serum lactate level trends and the postoperative management and course, with the special focus on the hemodynamic function of the transplanted heart.
Conclusions
Throughout the observation, all of the patients experienced at least one episode of hyperlactatemia, with the median peak value of 7.0 (4.5–8.4) mmol/L. Various serum lactate level trends can be identified in post-HTX patients, with the greatest differences in terms of the ICU admission measurement, and the highest observed value. Further research is required to determine the clinical usefulness of newly reported serum lactate level trends among heart transplant recipients.