Gastroduodenal artery aneurysm/ pseudoaneurysm: a systematic review of reported cases
- Published
- Accepted
- Received
- Academic Editor
- Sonia Oliveira
- Subject Areas
- Emergency and Critical Care, Gastroenterology and Hepatology, Surgery and Surgical Specialties
- Keywords
- Gastroduodenal artery, Visceral artery aneurysm, Clinical manifestation, Intervention, Outcome
- Copyright
- © 2025 Lee et al.
- Licence
- This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits using, remixing, and building upon the work non-commercially, as long as it is properly attributed. For attribution, the original author(s), title, publication source (PeerJ) and either DOI or URL of the article must be cited.
- Cite this article
- 2025. Gastroduodenal artery aneurysm/ pseudoaneurysm: a systematic review of reported cases. PeerJ 13:e19115 https://doi.org/10.7717/peerj.19115
Abstract
Background
This systematic review and meta-analysis investigated the clinical characteristics of patients with gastroduodenal artery aneurysm (GDA), identified risk factors associated with poor clinical outcomes, and elucidated potential differences between various GDA etiologies.
Methods
A systematic literature search was conducted from January 2000 to October 2023 in the PubMed, EMBASE, and Google Scholar databases. The analysis focused on extracting data regarding clinical presentations, diagnostic modalities, and patient outcomes.
Results
This meta-analysis included data from 224 patients derived from 207 case reports spanning 47 countries over a 23-year period. The majority of patients presented with comorbidity (85.3%) and had a predisposing factor for GDA (71.9%). The diagnostic accuracy of the three most common diagnostic investigations—namely angiography, abdominal computed tomography, and ultrasound—was 100.0%, 86.2%, and 59.6%, respectively. Transarterial embolization (75.0%) and surgery (24.1%) were the two most common therapeutic approaches. Emergent treatment for GDA was necessary in 31.7% of patients. Notably, hemostasis was achieved after the initial treatment attempt in 82.6% of patients. The in-hospital mortality rate was 6.7%, with complications occurring in 16.1% of cases. A higher percentage of patients with a complicated hospital course were subjected to observation management and presented with shock during hospitalization.
Conclusions
Patients with GDA often have comorbidities and predisposing factors. Clinical presentations of GDA were found to include abdominal pain, hemorrhage, and obstruction of peripheral structures in the vicinity of the gastroduodenal artery. Splanchnic artery angiography and abdominal computed tomography are recognized as the most accurate tools for diagnosing GDA. Endovascular management is the mainstay treatment approach for most patients and have a high rate of hemostasis success during the initial intervention. Surgical intervention is also a practical treatment. Conservative management with observation management may lead to a complicated hospital course, highlighting the potential benefit of aggressive treatment strategies for GDA. Patients with pancreatitis exhibited more comorbidities, predisposing factors, and a broader spectrum of clinical manifestations compared to those without pancreatitis. However, the in-hospital mortality rate was lower in the pancreatitis group, likely due to the younger age of the patients and the more prominent clinical presentations, which prompted earlier and more extensive diagnostic imaging studies.
Introduction
Gastroduodenal artery aneurysm/pseudoaneurysm (GDA) is a rare but life-threatening vascular abnormality (Corey et al., 2016; Maeno et al., 2022; Brodie & Kocher, 2019). Clinical manifestations of GDA often lack specificity, and the rupture rate in GDA surpasses that in other visceral artery aneurysms (VAAs) (Corey et al., 2016; Shukla et al., 2015). Notably, rupture of a VAA is associated with a significantly increased mortality rate (Corey et al., 2016; Shukla et al., 2015). Therefore, health-care professionals must comprehensively understand the common clinical presentations, appropriate diagnostic tools, and effective management strategies for GDA.
Studies on patients with GDA as a distinct group are limited. These patients are often grouped within broader investigations of VAAs (Barrionuevo et al., 2020; Gabrielli et al., 2017; Pitton et al., 2015). However, VAAs can manifest in various arterial locations, including hepatic, renal, splenic, celiac, gastric, gastroepiploic, jejunal, colic, superior mesenteric, gastroduodenal, and pancreaticoduodenal arteries (Barrionuevo et al., 2020; Pitton et al., 2015). The diverse clinical presentations associated with each VAA location and etiology hinder a clear understanding of GDA, specifically when data are aggregated across all VAAs.
Due to the low incidence of GDA, conducting large randomized controlled trials on this topic is challenging. Observational, real-world data can provide valuable insights into GDA. Numerous case reports and series have described the management approaches for patients with GDA (Gupta et al., 2018; Lazzara et al., 2021; Priya et al., 2016). However, these reports have often focused on specific etiologies such as pancreatitis, abdominal surgeries, and invasive abdominal procedures, limiting their generalizability. To address this gap, we conducted a comprehensive systematic review to investigate in detail the clinical manifestations of patients with GDA.
The objective of this systematic review and meta-analysis was to investigate the clinical characteristics of patients with GDA, identify risk factors associated with poor clinical outcomes, and elucidate potential differences between the various etiologies of GDA.
Survey methodology
Study selection and data extraction
This systematic review was conducted in accordance with a preregistered protocol (PROSPERO: CRD42023487443) and adhered to the Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) reporting guidelines. A comprehensive literature search was conducted from January 2000 to October 2023 in the PubMed, EMBASE, and Google Scholar databases. Additionally, reference lists of potentially eligible studies were screened to identify further relevant articles. No language or country restrictions were imposed. Non-English manuscripts were translated using Google Translate (Mountain View, CA, USA).
The search strategy employed the keywords “gastroduodenal artery aneurysm” and “gastroduodenal artery pseudoaneurysm”. Two authors (YTL and KTC) independently assessed titles and abstracts retrieved from the search. Pertinent manuscripts were selected for full-text review. Because no randomized controlled trials or large retrospective studies on GDA were identified during the preliminary search, case series and case reports featuring patients with GDA were included. These included studies had to provide detailed information on four key aspects: clinical manifestations of GDA, diagnostic tools employed, GDA management strategies, and patient prognosis. Unpublished research, conference communications, inaccessible articles, and case reports lacking essential details were excluded from the analysis.
The following data were extracted from the included articles: first author name, publication year, country of origin, patient characteristics, clinical manifestations, diagnostic tools employed, GDA management approaches, treatment effects, in-hospital mortality rates, and any reported complications. Any discrepancy arising during data extraction was resolved through consensus between reviewers (YHL and KTC). If consensus could not be reached, final arbitration was provided by CCH.
Data analysis and group comparisons
The patients in the included studies were categorized into distinct groups to enable comparisons. First, we compared patients who experienced a complicated hospital course (defined as in-hospital mortality or posttreatment complications) with those without such complications. Second, given that pancreatitis is the most prevalent comorbidity associated with GDA, we compared patients with and without pancreatitis.
Statistical analyses were performed using SPSS 15 (SPSS, Chicago, IL, USA). Categorical data are presented as frequencies and percentages, whereas continuous data such as age and GDA size are presented as medians within interquartile ranges (IQRs). The Mann–Whitney U test was employed to assess differences in age and GDA size between groups. For categorical data, intergroup comparisons were performed utilizing the chi-square test.
Results
Search for and identification of studies
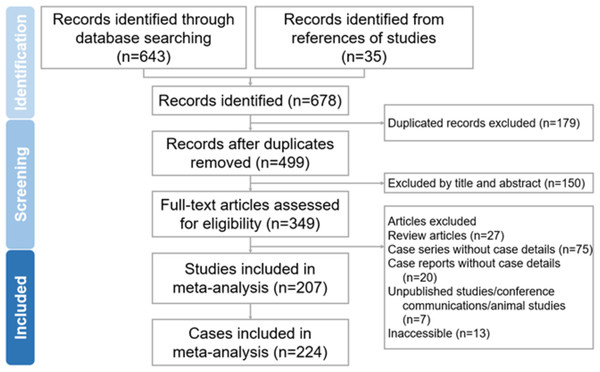
A total of 643 citations were initially retrieved from the database search, with an additional 35 citations obtained from the reference lists of relevant studies. Of these, 179 citations were excluded due to duplication, and 150 citations were excluded on the basis of title and abstract screening. This resulted in 349 citations selected for a detailed evaluation. Following a meticulous assessment, 142 articles were further excluded: 27 review articles, 75 case series, and 20 case reports lacking essential patient details. Additionally, seven unpublished studies, conference communications, and animal studies, along with 13 articles that were inaccessible, were excluded from the analysis. Consequently, this meta-analysis included 207 case reports and case series, encompassing data from a total of 224 patients. Figure 1 illustrates the PRISMA flow diagram for the search and identification of included studies.
Figure 1: Preferred reporting items for systematic reviews and meta-analysis flow diagram for the search and identification of included articles.
Characteristics of enrolled patients
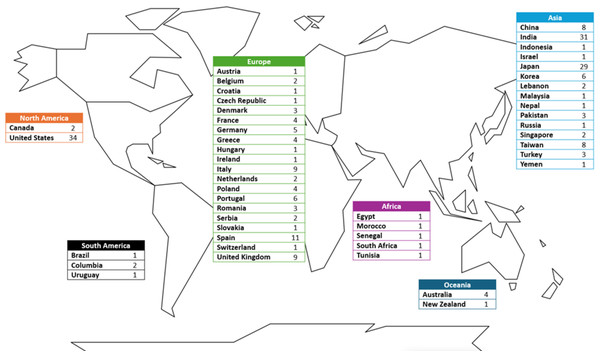
Figure 2 depicts the geographic distribution of reported cases. Data originated from patients in 47 countries in all continents, with the United States, India, and Japan constituting 42.0% of all included cases. Of the 224 patients included in this analysis, 221 had documented age data, and the median age was 33.5 years (IQR: 29–39 years). Notably, five case reports lacked information on patient sex. Among the remaining cases, male predominance was observed, with men accounting for 71.2% of the cohort. The majority of patients presented with a comorbidity (85.3%) and had a predisposing factor for GDA (71.9%). These predisposing factors were pancreatitis (Klauß et al., 2012); prior gastrointestinal, biliary, or pancreatic surgery (Moore et al., 2004); percutaneous or internal drainage of abdominal lesion (Basile et al., 2002); intra-abdominal tumor (Androulakakis et al., 2001); peptic ulcer disease (Maggiore, 2001); infectious disease (Sinduja et al., 2021); trauma (Babu et al., 2016); the use of anticoagulants (Harris, Chalhoub & Koirala, 2010); and others (including median arcuate ligament syndrome, systemic lupus erythematosus, hemophilia, and polyarteritis nodosa) (Jensen et al., 2020; Hoorn et al., 2011; Nouira et al., 2006; Dönmez et al., 2005). Data on GDA size were available for 62% of patients, with the median size found to be 3.0 cm (IQR: 2.0–5.0 cm).
Figure 2: Geographic distribution of reported cases.
Data include cases from 47 countries across all continents.Clinical manifestations and diagnostic tools
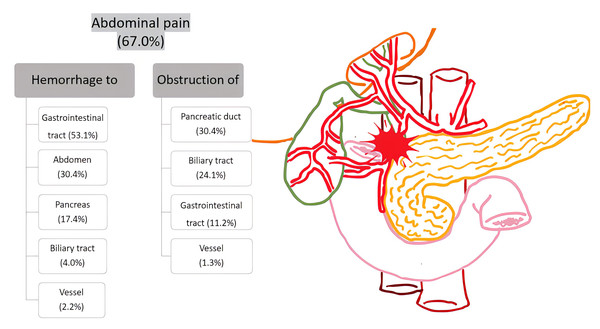
Abdominal pain (67.0%) was the most prevalent presentation of GDA. Other clinical manifestations were categorized as bleeding in the gastrointestinal tract, abdomen, pancreas, biliary system, or vessels; obstruction in the gastrointestinal tract, pancreatic duct, biliary system, or vessels; and miscellaneous symptoms (Fig. 3). The lesions on the vessels involved either hemorrhage or compression affecting the superior mesenteric vein, portal vein, common hepatic artery, and inferior vena cava. These symptoms could be directly caused by GDA or related to factors associated with GDA.
Figure 3: Clinical manifestations of GDA
The three most common presentations are abdominal pain, hemorrhage, and obstruction of internal organs.Abdominal computed tomography scans were found to be the primary diagnostic tool; they were employed in 87.5% of patients and had high diagnostic accuracy of 86.2%. Angiography served a dual role as both a diagnostic tool (employed in 90.2% of patients; accuracy: 100%) and a treatment modality. Abdominal or endoscopic ultrasound was frequently employed for evaluating abdominal lesions, but with low diagnostic accuracy (56.9%). Notably, extraluminal protruding masses and hemorrhage from the ampulla of Vater were identified as endoscopic findings associated with GDA (Giri, Angadi & Bhrugumalla, 2022; Yoshida et al., 2020). GDA-related findings were observed in 23.4% of gastrointestinal endoscopic examinations. Additionally, endoscopic retrograde cholangiopancreatography (9.8%), magnetic resonance imaging (7.6%), and red blood cell scintigraphy (0.9%) were less frequently employed for diagnosis than were other methods. Vascular abnormalities other than GDA were discovered in 19.2% of patients.
GDA management approaches and prognosis
This review included 66 true aneurysm and 158 pseudoaneurysm. Treatment for GDA was conducted emergently in 31.7% of patients, with 34.8% experiencing shock during hospitalization. Transarterial embolization (TAE; 75.0%) and surgery (24.1%) were the primary treatment modalities. Percutaneous thrombin injection (6.7%), vascular stenting (4.5%), and observation (2.7%) were also employed for GDA management. Endovascular managements, including TAE, percutaneous thrombin injection, and vascular stenting, comprised 193 (86.2%) of treatment options. The gastroduodenal artery is part of the collateral network between the celiac trunk and the superior mesenteric artery territories. Therefore, embolization of the GDA in such cases carries the risk of visceral ischemia due to the potential loss of vital collateral blood flow. In this study, we identified one patient with congenital absence of the celiac trunk, one with occlusion of the celiac trunk, three with stenosis of celiac trunk, and one with stenosis of superior mesenteric artery. Among these, the first two patients underwent surgery, while the remaining four underwent TAE. All six patients were successfully treated without sequelae of visceral ischemia.
Regarding prognosis, hemostasis was achieved in 82.6% of patients at the initial treatment attempt. The in-hospital mortality rate was 6.7%, with complications occurring in 16.1% of cases. The mortality rate is higher in patient with true aneurysm (12.1%) than those with pseudoaneurysm (4.3%). Table 1 presents the characteristics, diagnostic tools, treatment strategies, and prognosis of the reviewed cases.
| Characteristics | Treatments for GDA | ||
|---|---|---|---|
| Age (year)* | 55.0 (42.0–68.0) | TAE | 75.0% |
| Male | 71.2% | Surgery | 24.1% |
| Comorbidity | 85.3% | Thrombin injection | 6.7% |
| Predisposing factor | 71.9% | Vascular stent | 4.5% |
| Size of GDA (cm)* | 3.0 (2.0–5.0) | Observation | 2.7% |
| Diagnostic tools | Prognosis | ||
| CT | 84.8% | Shock during hospitalization | 34.8% |
| Non-diagnostic CT | 12.5% | Emergent treatment for GDA | 31.7% |
| Angiography | 90.2% | Hemostasis in initial treatment | 82.6% |
| Ultrasound | 17.9% | In-hospital mortality | 6.7% |
| Non-diagnostic ultrasound | 13.8% | Complication | 16.1% |
| Endoscopy | 11.6% | Additional vascular abnormality | 19.2% |
| Non-diagnostic endoscopy | 33.5% | ||
| MR | 7.6% | ||
| ERCP | 9.8% | ||
| RBC scintigraphy& | 0.9% | ||
Notes:
- GI
-
gastrointestinal tract
- CT
-
computed tomographic scan of abdomen
- MR
-
magnetic resonance
- ERCP
-
endoscopic retrograde cholangiopancreatography
- RBC
-
red blood cell
- TAE
-
transarterial embolization
Comparison of the complicated and uncomplicated hospital course groups
Table 2 presents a comparison of patients with complicated versus uncomplicated hospital courses. The two groups had similar characteristics. Regarding clinical manifestations, the complicated hospital course group had higher incidences of bleeding in the peritoneum/retroperitoneum, gastrointestinal obstruction, and biliary obstruction than did the uncomplicated hospital course group (complicated vs. uncomplicated: bleeding to peritoneum and retroperitoneum: 46.5% vs. 26.5%, p = 0.010; gastrointestinal obstruction: 23.3% vs. 8.3%, p = 0.005; biliary obstruction: 37.2% vs. 21.0%, p = 0.025, respectively). Compared with patients in the uncomplicated hospital course group, those with a complicated hospital course underwent fewer TAE procedures, were under observation more frequently, and were more likely to experience shock during hospitalization (complicated vs. uncomplicated: TAE: 62.8% vs. 77.9%, p < 0.001; observation: 11.6% vs. 0.6%, p < 0.001; shock during hospitalization: 51.2% vs. 34.8%, p = 0.012).
| Complicated (43) | Uncomplicated (181) | p | |
|---|---|---|---|
| Characteristics | |||
| Age (year)* | 55.5 (47.5–67.0) | 55.0 (41.0–68.0)* | 0.350 |
| Male | 78.0% | 69.7% | 0.285 |
| Comorbidity | 90.7% | 84.0% | 0.264 |
| Predisposing factor | 72.1% | 71.8% | 0.972 |
| Size of GDA (cm)* | 2.7 (1.5–5.5) | 3.0 (2.0–5.0)* | 0.516 |
| Clinical manifestations | |||
| Abdominal pain | 74.4% | 65.2% | 0.248 |
| Bleeding to GI tract | 46.5% | 54.7 | 0.334 |
| Bleeding to abdomen | 46.5% | 26.5 | 0.010 |
| Bleeding to pancreas | 11.6% | 18.8% | 0.266 |
| Bleeding to biliary tract | 4.7% | 3.9% | 0.684 |
| Bleeding to vessel | 0.0% | 2.8% | 0.586 |
| GI obstruction | 23.3% | 8.3% | 0.005 |
| Pancreatic duct obstruction | 30.2% | 30.4% | 0.984 |
| Biliary obstruction | 37.2% | 21.0% | 0.025 |
| Vessel obstruction | 2.3% | 1.1% | 0.474 |
| Additional vascular abnormality | 14.0% | 12.2% | 0.331 |
| Treatments for GDA | |||
| TAE | 62.8% | 77.9% | 0.000 |
| Surgery | 30.2% | 22.7% | 0.296 |
| Thrombin injection | 2.3% | 07.7% | 0.202 |
| Vascular stenting | 2.4% | 5.0% | 0.450 |
| Observation | 11.6% | 0.6% | 0.000 |
| Prognosis | |||
| Shock during hospitalization | 51.2% | 34.8% | 0.012 |
| Emergent treatment for GDA | 44.2% | 31.7% | 0.050 |
| Hemostasis in initial treatment | 81.4% | 82.9 | 0.818 |
Notes:
- GI
-
gastrointestinal tract
- TAE
-
transarterial embolization
Comparison of patients with versus without pancreatitis
We identified 102 (45.5%) patients with pancreatitis, of which 78 had chronic pancreatitis and 24 had acute pancreatitis. Patients with pancreatitis and those without were significantly different in their characteristics and clinical presentations. Patients with pancreatitis tended to be younger, were more likely to be male, and had more comorbidities and predisposing factors. In terms of clinical presentations, abdominal pain, bleeding (gastrointestinal, pancreatic, and biliary), and pancreatic duct and biliary obstructions were all significantly more prevalent in the patients with pancreatitis than in those without. Additionally, thrombin injection was more frequently administered to patients with pancreatitis, and vascular stenting was not applied in this group. Notably, a higher proportion of patients without pancreatitis experienced shock and in-hospital mortality compared with those with pancreatitis. Table 3 presents a detailed comparison of these findings.
| Pancreatitis (102) | Non-pancreatitis (122) | p | |
|---|---|---|---|
| Characteristics | |||
| Age (year)* | 49.5 (39.0–62.0) | 61.0 (46.0–71.0)* | 0.000 |
| Male | 83.0% | 61.3% | 0.022 |
| Comorbidity | 97.1% | 75.4% | 0.000 |
| Predisposing factor | 100.0% | 48.4% | 0.000 |
| Size of GDA (cm)* | 3.0 (2.2–5.0) | 3.0 (1.7–5.0)* | 0.173 |
| Clinical manifestations | |||
| Abdominal pain | 74.5% | 48.4% | 0.000 |
| Bleeding to GI tract | 59.8% | 38.5% | 0.002 |
| Bleeding to abdomen | 19.6% | 10.7% | 0.060 |
| Bleeding to pancreas | 26.5% | 5.7% | 0.000 |
| Bleeding to biliary tract | 3.9% | 0.0% | 0.042 |
| Bleeding to vessel | 4.9% | 9.0% | 0.234 |
| GI obstruction | 13.7% | 13.1% | 0.894 |
| Pancreatic duct obstruction | 51.0% | 18.9% | 0.000 |
| Biliary obstruction | 31.4% | 0.0% | 0.000 |
| Vessel obstruction | 2.9% | 0.0% | 0.091 |
| Additional vascular abnormality | 17.6% | 20.5% | 0.590 |
| Treatments for GDA | |||
| TAE | 76.5% | 73.8% | 0.642 |
| Surgery | 22.5% | 25.4% | 0.618 |
| Thrombin injection | 12.7% | 1.6% | 0.001 |
| Vascular stenting | 0.0% | 8.2% | 0.002 |
| Observation | 1.0% | 4.1% | 0.215 |
| Prognosis | |||
| Shock during hospitalization | 26.5% | 41.8% | 0.016 |
| Emergent treatment for GDA | 25.5% | 36.9% | 0.068 |
| Hemostasis in initial treatment | 84.3% | 81.1% | 0.534 |
| In-hospital mortality | 2.9% | 9.8% | 0.042 |
| Complication | 19.6% | 13.1% | 0.188 |
Notes:
- GI
-
gastrointestinal tract
- TAE
-
transarterial embolization
Bias
Due to the retrospective study design and heterogeneity of clinical parameters in the included studies, a high risk of bias was noted, which may result in the drawing of weak conclusions.
Discussion
The study revealed a male predominance (71.2%) among patients with GDA and that these patients frequently presented with comorbidities (85.3%) and predisposing factors (71.9%). Nearly half of the patients with GDA had coexisting pancreatitis, a condition known for its male predominance and frequent association with intra-abdominal complications (Klauß et al., 2012; Vege & Chari, 2022). Although idiopathic GDA exists, these findings highlight the importance that health-care professionals consider the possibility of GDA during diagnostic workup, particularly when a patient has predisposing factors.
Although most clinical manifestations of GDA are nonspecific and can be attributed to predisposing factors such as pancreatitis or other intra-abdominal pathologies, three key features were identified: abdominal pain, hemorrhage into surrounding structures, and obstruction of adjacent organs such as the abdomen, the gastrointestinal tract, the pancreas, the biliary system, and vascular structures. If management for established intra-abdominal pathologies fails to achieve clinical resolution, vascular lesions such as GDA in the vicinity should be investigated.
Splanchnic artery angiography is the most accurate tool for diagnosing GDA (Habib et al., 2013). However, this approach is invasive and often necessitates antecedent imaging studies of suspect vascular lesions. For a comprehensive evaluation of both GDA presence and potentially predisposing intra-abdominal pathologies, abdominal computed tomography scans are recommended. Computed tomography scans offer accurate diagnosis of GDA and reveal the details of the anatomy surrounding the vessel. Ultrasounds, including both abdominal and endoscopic modalities, are commonly employed in initial examinations for intra-abdominal conditions due to their lack of radiation and contrast-agent-related toxicity (Piasek et al., 2018). However, their diagnostic yield for GDA is limited, particularly in emergent settings involving unprepared patients. Nevertheless, if an uncharacterized intra-abdominal cystic lesion is identified on ultrasound, Doppler ultrasound may reveal turbulent blood flow within the lesion, raising suspicion of an aneurysm. Endoscopy is a common procedure for patients presenting with abdominal pain and gastrointestinal hemorrhage, both of which are characteristic presentations of GDA. During endoscopy, health-care professionals should be attentive to specific findings suggestive of GDA, such as extraluminal protruding masses or hemorrhage from the ampulla of Vater. These findings warrant further investigation for GDA.
More than one-third of the included patients experienced a shock episode during hospitalization, with 31.7% patients requiring emergent treatment; these findings emphasize the critical need for prompt diagnosis and intervention in GDA. Endovascular management, including transarterial embolization, percutaneous thrombin injection, and placement of a vascular stent, was the primary treatment strategy for most patients. Surgical intervention was employed in approximately one-fourth of cases. Notably, timely diagnosis and appropriate treatment for GDA resulted in successful hemostasis at the initial intervention in 82.6% of patients, highlighting the potential for effective management of life-threatening GDA. A retrospective study comparing intact and ruptured visceral artery aneurysms found that patients with ruptured aneurysms had a higher percentage of pseudoaneurysms compared to those with intact aneurysms (Shukla et al., 2015). However, the management principles for visceral artery aneurysms and pseudoaneurysms are similar.
An analysis of baseline characteristics revealed no significant differences between patients with complicated and those with uncomplicated hospital courses. Notably, the complicated hospital course group had a higher proportion of patients managed through observation than the uncomplicated hospital course group did. Additionally, the complicated hospital course group had a higher proportion of patients who experienced shock during hospitalization. However, despite these factors potentially indicating a more critical clinical state and a trend toward more emergent treatment, the rates of hemostasis in the two groups were comparable. These findings suggest that aggressive treatment approaches for GDA may be warranted, instead of palliative care.
Patients with coexisting pancreatitis exhibited a broader spectrum of clinical manifestations compared with those without pancreatitis. However, the in-hospital mortality rate was lower in the pancreatitis group. This improved prognosis may be attributable to two factors. First, patients with pancreatitis tended to be younger than their counterparts without pancreatitis. Second, the more prominent clinical presentation in the pancreatitis group may have prompted more comprehensive diagnostic workup, potentially leading to incidental identification of GDA in imaging studies. Early diagnosis of GDA in the pancreatitis group may have translated to a lower incidence of shock during hospitalization. The possible pathogenic mechanisms of GDA and pancreatitis include progressive inflammation and enzymatic autodigestion of the peripancreatic artery, as well as a pseudocyst eroding a visceral artery (Klauß et al., 2012), both of which are common in patients with chronic pancreatitis. However, we observed that 23.5% of patients with pancreatitis-related GDA were caused by acute pancreatitis.
Strengths and limitations
This meta-analysis systematically reviewed data from 224 patients, derived from 207 case reports spanning 47 countries over a 23-year period. The inclusion of such a substantial number of patients enabled a comprehensive and detailed examination of individuals with GDA. The reviewed cases offer a diverse and global clinical perspective on patients with GDA, potentially offering valuable insights to health-care professionals worldwide.
However, several limitations of this meta-analysis should be acknowledged. First, the significant heterogeneity among the included studies, attributable to their diverse origins, limited our ability to analyze detailed hospital stay data for patients with GDA. Second, international variations in hospital resources and equipment precluded direct comparisons of treatment strategies and outcomes across the reviewed cases. Third, the influence of predisposing factors on the clinical presentations and outcomes of patients with GDA could not be fully elucidated due to the diverse nature of these factors. This heterogeneity may have contributed to distinct clinical courses among patients with GDA resulting from various causes. Finally, it is important to acknowledge the potential for survivorship bias in this review, as most case reports tend to present successfully treated cases.
Conclusions
Patients with GDA often have comorbidities and predisposing factors. Clinical presentations of GDA were found to include abdominal pain, hemorrhage, and obstruction of peripheral structures in the vicinity of the gastroduodenal artery. Splanchnic artery angiography and abdominal computed tomography are recognized as the most accurate tools for diagnosing GDA. Endovascular management is the mainstay treatment approach for most patients and have a high rate of hemostasis success during the initial intervention. Surgical intervention is also a practical treatment. Conservative management with observation management may lead to a complicated hospital course, highlighting the potential benefit of aggressive treatment strategies for GDA. Patients with pancreatitis exhibited more comorbidities, predisposing factors, and a broader spectrum of clinical manifestations compared to those without pancreatitis. However, the in-hospital mortality rate was lower in the pancreatitis group, likely due to the younger age of the patients and the more prominent clinical presentations, which prompted earlier and more extensive diagnostic imaging studies.