The efficacy comparison on femoral vein hemodynamics and morphology between two types of graduated elastic compression stockings among patients undergoing knee replacement: a single center, double-blind, randomized trial
- Published
- Accepted
- Received
- Academic Editor
- Ana Maria Jimenez-Cebrian
- Subject Areas
- Clinical Trials, Hematology, Internal Medicine, Orthopedics
- Keywords
- Graduated elastic compression stockings, Knee replacement, DVT, Prophylaxis
- Copyright
- © 2025 Xu et al.
- Licence
- This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits using, remixing, and building upon the work non-commercially, as long as it is properly attributed. For attribution, the original author(s), title, publication source (PeerJ) and either DOI or URL of the article must be cited.
- Cite this article
- 2025. The efficacy comparison on femoral vein hemodynamics and morphology between two types of graduated elastic compression stockings among patients undergoing knee replacement: a single center, double-blind, randomized trial. PeerJ 13:e19070 https://doi.org/10.7717/peerj.19070
Abstract
Background
Venous thromboembolism is a significant complication after knee replacement. The short-term efficacy disparities between different types of graduated elastic compression stockings (GCS) among patients undergoing total/unicompartmental knee replacement remain unclear.
Objective
The aim of the trial was to compare the efficacies on hemodynamics and morphology of femoral vein between two types of GCS, providing more evidence on GCS prophylaxis among patients undergoing total/unicompartmental knee replacement.
Methods
In this single center, double-blind, parallel design, randomized trial, 141 adult patients who underwent selective, unilateral total/unicompartmental knee replacement operation for the first time were enrolled, with 71 were assigned to type A GCS and 70 to type B GCS, respectively. Compressed ultrasound of the lower extremity was conducted before the operation (without GCS, as preoperative baseline) and within 24 hours post operation (postoperative baseline , with GCS, and with GCS + ankle pump). The relative changes in TV and PV, as well as the diameter of the femoral vein in the healthy leg, were assessed both before and after GCS application following the knee replacement surgery.
Results
The median ages were 67.0 years in type A group and 68.0 years in type B group. All parameters of femoral vein were comparable between type A and type B GCSs. Compared with postoperative baseline, GCS + ankle pump significantly reduced femoral vein diameter and improved the TV in both GCS types; GCS and GCS + ankle pump also significantly increased the TV (median 1.2%, IQR −21.4% to 58.6%, P = 0.0384; median 14.0%, IQR −24.3% to 93.0%, P = 0.0019, respectively) in left leg, while not significant in right leg.
Conclusion
The efficacies of two GCSs were comparable, and both were effective in improving velocity and morphology of femoral veins of the healthy legs among patients undergoing knee replacement, especially in improving TVs of femoral veins for left leg.
Introduction
Venous thromboembolism (VTE) is a common complication after knee replacement. The reported incidence of deep vein thrombosis (DVT) in patients without prophylaxis was 40% to 84% after knee replacement (Cohen et al., 1973; Lynch et al., 1988; O’Reilly, Burgess & Zicat, 2005; Stringer et al., 1989; Stulberg et al., 1984). Even if the true morbidity and mortality rates of untreated DVT are unknown (Cho et al., 1998), the prevalence of pulmonary embolism (PE) ranged from 1.8% to 7%, significantly increasing the risk of in-hospital mortality (Leclerc et al., 1998; Wells et al., 1995). All components of Virchow’s triad are typically present after knee replacement: (1) venous stasis due to tourniquet use and immobilization; (2) vascular endothelial injuries caused by surgical manipulations; (3) hypercoagulability from trauma and application of polymethylmethacrylate bone cement (Flevas et al., 2018). In light of these risk factors, both pharmacological and mechanical prophylaxis have been strongly recommended for patients undergoing knee replacement by guidelines, with a DVT reduction to around 10% (Falck-Ytter et al., 2012; Trc, Kvasnicka & Kudrnová, 2007). Mechanical prophylactic strategies, mainly including graduated elastic compression stocking (GCS), intermittent pneumatic compression (IPC) and ankle pump, are recommended especially for the patients with high risk of bleeding (Flevas et al., 2018). The advantages of mechanical prophylaxis include the minimal risk of bleeding, no need for laboratory monitoring and the absence of clinically important side effects.
GCS stimulate blood flow by applying differential pressure to the legs, reducing DVT by 57% after total hip arthroplasty (MacLellan & Fletcher, 2007). Considering efficacy and convenience, GCS has been widely recommended for prophylaxis of DVT. However, an inappropriate pressure gradient may reduce the prophylactic efficacy and even cause complications due to impairment in tissue oxygenation (Agu, Hamilton & Baker, 1999). Certain effects on hemodynamics among patients after knee replacement have not been studied. Our previous polit study among healthy volunteers demonstrated difference on effects to the deep veins between different types of GCS (Yang et al., 2023), but conditions in post-surgical patients vary significantly due to factors like systemic stress and endothelial injury.
Thus, we conducted a randomized control trial to compare the efficacy of two types of GCS with different graduated pressures on hemodynamics and morphology of femoral veins in patients undergoing knee replacement surgery. This study aimed to provide more evidence on the efficacy and underlying mechanism of GCS prophylaxis in this population.
Material and Methods
Study design and participants
This was a single center, double-blind, parallel design, randomized trial, conducted from August 10th to December 31st in 2023, adult patients who underwent selective, unilateral total/unicompartmental knee replacement for the first time and did not have any predisposition to VTE were prospectively enrolled. Those with a previous history of either varicose veins or peripheral vascular disease, skin ulcers, dermatitis, wounds or VTE, preoperative prolonged immobilization or limited movement of lower limbs were excluded. The study was approved by the institution ethics board of China-Japan Friendship Hospital (2023-KY-130) and written informed consent was obtained from each patient. The study protocol was registered at Chinese Clinical Trial Registry website (http://www.chictr.org.cn/, registration number: ChiCTR2300074136; registration date: July 31st, 2023).
Randomization
Eligible patients were randomly assigned to type A or B GCS group by a 1:1 ratio through a randomization table generated by SAS 9.4 software (Cary, NC, USA). The group number was sealed in a light-tight envelope and was blind for both researchers and patients. Investigators who measured the outcome and statisticians who performed statistical analysis were also blind to the group assignment.
Assessment
The assessments have been described in our previous study (Yang et al., 2023). Briefly, the graduated compressions of type A GCS were as follows: eight mmHg-ankle, 13 mmHg-crus, 10 mmHg-popliteal fossa, eight mmHg-middle thigh and six mmHg-upper thigh. The graduated compressions of type B GCS were as following: eight mmHg-ankle, 14 mmHg-crus, eight mmHg-popliteal fossa, eight mmHg-middle thigh and six mmHg-upper thigh. The dimensions for the GCS type were selected according to the measuring chart recommended by the manufacturer (Zhende Medical Co., Ltd., Shaoxing, China).
Compressed ultrasound of the lower extremity was conducted before the operation (without GCS, as preoperative baseline) and within 24 h post operation (postoperative baseline, with GCS, and with GCS + ankle pump) on the heathy leg, because the leg which underwent knee replacement would be unable to wear GCS. The postoperative baseline was measured at least half an hour later after the patient returned to the ward. Similarly, measurements of the efficacy of GCS or GCS + ankle pump were also required at least half an hour’s intervals after wearing GCS or with ankle pump movement. Before and during the examination, all participants were asked to lie in the supine position, keep their emotions calm and limbs relaxed, and breath as steady as possible, since the blood flow velocity might be influenced by their breath.
Blood flow velocity and diameters of the femoral vein in healthy legs were assessed using a Doppler ultrasound scanner (Mindray Resona 8 Colour Doppler Equipment; Mindray Co, Shenzhen, China) equipped with a 7–10 MHz linear probe (SuperLinear 14-5; Mindray Co, Shenzhen, China). Measurements were conducted by a single experienced sonographer. Peak velocity (PV, cm/s) and trough velocity (TV, cm/s) of the femoral veins were assessed in four different conditions for each participant: lying down, during ankle pump exercises, with GCS alone, and with GCS while performing ankle pump movements. The probe was placed longitudinally regarding the axis of the vein, maintaining about two mm distance from the skin to reduce compression effects on the vein. The Doppler ultrasound was set to pulsed mode, maintaining an incident angle below 60°, with the sampling volume aligned parallel with blood flow to encompass the center of the venous lumen. The pulse repetition frequency was set between 603–1500 Hz. To ensure higher measurement reliability, once the signal was stable, five images were frozen and averaged for each participant.
Outcomes
The primary outcome was the relative change of TV in femoral vein of the healthy leg after knee replacement operation before and after wearing GCS. The secondary outcomes were the relative changes of diameter and PV of femoral vein in differences between two types of GCS.
Statistical analysis
According to the result of our pilot study (Yang et al., 2023), a trough of 126 patients were necessary to meet the statistical power of 80% at a two-sided significance level of 0.05. If only 90% of patients enrolled in the trial were included in the primary analysis, the sample size was expanded to 140. The full analysis set (FAS) including patients who underwent randomization and were capable for GCS and compressed ultrasound after operation were analyzed. In this study, the per protocol set (PPS) and the safety set (SS) were the same set as FAS. No adverse event was found during the study period. The relative changes of femoral vein parameters were calculated as:
Relative change (%) = .
Timepoint B refers to a latter timepoint, such as GCS or GCS + ankle pump, timepoint A refers to a prior timepoint, such as preoperative or postoperative.
A positive value of relative change referred to the improvement of parameter value and a negative value referred to the decline of parameter value of femoral vein.
In addition to the comparisons between two types of GCS, a further comparison of the efficacy differences between the left and the right healthy legs among the entire participants was conducted, regardless of GCS types. The before-and-after comparisons were also performed to verify the efficacy of interventions (GCS and GCS + ankle pump) in this study. Numerical variables were summarized as median (interquartile range (IQR)) and categorical variables were expressed as numbers and percentages, and differences between groups were compared using Wilcoxon rank-sum test or chi-square test/Fisher’s exact test, where appropriate. For the paired data within each group, like parameters before and after wearing GCS, Wilcoxon signed rank test was performed. All statistical analysis were performed using SAS 9.4 software (Cary, NC, USA) and a P value <0.05 was considered statistically significant.
Results
Characteristics of the participants
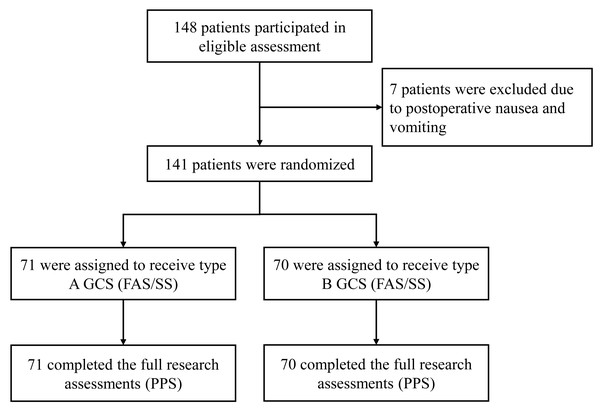
As is shown in the flowchart, a total of 148 patients underwent screening for eligibility for the study. Seven patients were unable to wear GCS and took following measurements due to postoperative nausea and vomiting and were excluded from the study. Finally, 141 patients were randomized and of whom, 71 were assigned to type A GCS and 70 to type B GCS, respectively. All patients who received randomization completed the study (Fig. 1).
Figure 1: Study flowchart of this study.
The median ages were 67.0 (interquartile range (IQR) 63.0, 71.0) years old in type A GCS group and 68.0 (IQR 60.0, 74.0) years old in type B GCS group. The body mass index (BMI), systolic blood pressure and diastolic blood pressure were comparable between two groups. The median PV and median TV of femoral vein were faster in patients with type A GCS than those with type B GCS (max 14.3 cm/s vs 12.3 cm/s, p = 0.0351; min 6.4 cm/s vs 4.8 cm/s, p = 0.0139). The median diameter of femoral vein was also smaller in patients with type A GCS (9.9 mm vs 11.0 mm, p = 0.0163) (Table 1).
| Characteristics | Type A GCS N = 71 | Type B GCS N = 70 | P |
|---|---|---|---|
| Demographics | |||
| Age, years | 67.0 (63.0, 71.0) | 68.0 (60.0, 74.0) | 0.8770 |
| BMI, Kg/m2 | 26.9 (24.7, 30.1) | 27.8 (25.0, 30.4) | 0.3482 |
| SBP, mmHg | 134.0 (120.0, 143.0) | 134.0 (127.0, 145.0) | 0.3262 |
| DBP, mmHg | 76.0 (70.0, 85.0) | 77.5 (74.0, 85.0) | 0.2488 |
| Parameters at rest (lie down) | |||
| FVp, cm/s | 14.3 (11.4, 18.4) | 12.3 (10.7, 16.3) | 0.0351 |
| FVt, cm/s | 6.4 (3.3, 9.6) | 4.8 (2.3, 7.4) | 0.0139 |
| FD, mm | 9.9 (9.0, 11.3) | 11.0 (9.5, 12.0) | 0.0163 |
Notes:
The compressed ultrasound of the lower extremity was conducted on the healthy leg in the supine position. Data were described as median (interquartile range).
- GCS
-
graduated compression stocking
- BMI
-
body mass index
- SBP
-
systolic blood pressure
- DBP
-
diastolic blood pressure
- FVp
-
peak velocity of femoral vein
- FVt
-
trough velocity of femoral vein
- FD
-
diameter of femoral vein
Primary and secondary outcomes of type A and B GCS
According to Table 2, no significant difference was observed between two groups on the relative change of TV in femoral vein of the healthy leg after knee replacement operation before and after wearing GCS. All the other parameters were comparable between type A and type B GCSs (Table 2).
| Relative change, % | Type A GCS N = 71 | Type B GCS N = 70 | P |
|---|---|---|---|
| Primary outcome† | |||
| GCS to postoperative baseline | 1.1 (−24.1, 47.1) | −0.6 (−21.7, 52.1) | 0.9441 |
| Secondary outcome | |||
| Diameters of femoral vein | |||
| Postoperative to preoperative baseline | −3.9 (−12.4, 6.4) | −4.3 (−13.4, 6.3) | 0.8641 |
| GCS to preoperative baseline | −12.2 (−21.6, −1.9) | −13.8 (−23.5, −4.0) | 0.8062 |
| GCS to postoperative baseline | −8.5 (−19.4, 0.0) | −10.5 (−17.6, −3.4) | 0.8967 |
| GCS + ankle pump to preoperative baseline | −13.5 (−23.0, −0.9) | −13.9 (−23.1, −4.1) | 0.9277 |
| GCS + ankle pump to postoperative baseline | −10.0 (−19.6, 2.6) | −10.0 (−16.0, −1.3) | 0.9901 |
| GCS + ankle pump to GCS | 1.4 (−6.5, 6.3) | 0.0 (−4.1, 5.9) | 0.9343 |
| Peak velocity of femoral vein | |||
| Postoperative to preoperative baseline | 2.6 (−21.2, 24.7) | 12.0 (−22.0, 44.6) | 0.2383 |
| GCS to preoperative baseline | −0.2 (−23.3, 43.8) | 7.8 (−7.7, 44.3) | 0.2176 |
| GCS to postoperative baseline | 0.8 (−17.7, 20.6) | −0.6 (−19.8, 17.9) | 0.6771 |
| GCS + ankle pump to preoperative baseline | 0.5 (−28.2, 46.3) | 13.8 (−17.0, 42.9) | 0.4859 |
| GCS + ankle pump to postoperative baseline | 2.4 (−18.9, 30.4) | −5.7 (−18.3, 16.8) | 0.3731 |
| GCS + ankle pump to GCS | −0.5 (−10.6, 15.9) | −0.3 (−12.7, 13.8) | 0.7540 |
| Trough velocity of femoral vein | |||
| Postoperative to preoperative baseline | 30.9 (−24.0, 146.8) | 43.5 (−26.9, 185.5) | 0.7167 |
| GCS to preoperative baseline | 34.5 (−13.3, 149.5) | 63.3 (−7.5, 225.5) | 0.6680 |
| GCS + ankle pump to preoperative baseline | 51.7 (−10.9, 175.1) | 76.3 (−5.0, 172.5) | 0.4026 |
| GCS + ankle pump to postoperative baseline | 15.0 (−25.2, 85.6) | −0.6 (−24.9, 66.5) | 0.7198 |
| GCS + ankle pump to GCS | −3.3 (−13.7, 35.7) | 4.1 (−14.5, 25.1) | 0.9408 |
Notes:
Data were described as median (interquartile range). P values were estimated by Wilcoxon rank-sum test.
- GCS
-
graduated compression stocking
As for the before-and-after relative changes on parameters of femoral vein by GCS types in Table S1, knee replacement significantly impacted the blood stream in femoral vein by reducing diameter and improving TV and PV in both GCS types. Compared with postoperative baseline, GCS + ankle pump significantly constricted femoral veins and improved the TV in both GCS types, while GCS alone did not (Table S1).
Differences between legs
As is shown in Table 3, among enrolled patients, 61 patients accepted knee replacement on left leg and wore GCS on right leg, while 80 patients were on the contrary. For both legs, GCS and GCS + ankle pump significantly constricted femoral veins compared with postoperative baseline (all P < 0.0001). However, compared with postoperative baseline, GCS and GCS + ankle pump also significantly improved the TV (median 1.2%, IQR −21.4% to 58.6%, P = 0.0384; median 14.0%, IQR −24.3% to 93.0%, P = 0.0019, respectively) in left leg, while not in right leg (Table 3).
| Relative changes, % | Right leg N = 61 | P | Left leg N = 80 | P | Total N = 141 | P |
|---|---|---|---|---|---|---|
| Diameters | ||||||
| postoperative to preoperative baseline | −2.5 (−9.2, 7.9) | 0.3364 | −4.9 (−14.9, 5.7) | 0.0408 | −4.3 (−12.7, 6.3) | 0.0229 |
| GCS to preoperative baseline | −14.0 (−22.4, −8.2) | <.0001 | −11.3 (−22.1, −1.0) | <.0001 | −13.5 (−22.4, −3.6) | <.0001 |
| GCS to postoperative baseline† | −14.0 (−19.8, −7.0) | <.0001 | −6.7 (−13.0, 1.2) | <.0001 | −9.6 (−18.2, −1.7) | <.0001 |
| GCS + ankle pump to preoperative baseline | −13.8 (−23.7, −4.1) | <.0001 | −13.6 (−22.3, 0.5) | <.0001 | −13.8 (−23.0, −2.6) | <.0001 |
| GCS + ankle pump to postoperative baseline‡ | −13.4 (−21.1, −3.5) | <.0001 | −7.2 (−14.5, 2.1) | <.0001 | −10.0 (−17.1, 0.0) | <.0001 |
| GCS + ankle pump to GCS | 1.4 (−4.3, 7.2) | 0.5860 | 0.0 (−5.6, 4.5) | 0.9796 | 0.8 (−5.2, 5.9) | 0.7185 |
| Peak velocity | ||||||
| postoperative to preoperative baseline | 7.1 (−12.3, 22.9) | 0.1335 | 3.9 (−27.1, 54.6) | 0.0590 | 6.8 (−21.2, 32.2) | 0.0209 |
| GCS to preoperative baseline | 1.8 (−21.3, 45.5) | 0.1090 | 7.1 (−17.1, 41.6) | 0.0275 | 3.7 (−19.8, 43.8) | 0.0060 |
| GCS to postoperative baseline | −0.4 (−17.2, 16.5) | 0.6936 | 1.5 (−20.3, 19.3) | 0.7179 | 0.8 (−17.7, 18.7) | 0.5491 |
| GCS + ankle pump to preoperative baseline | 10.4 (−22.9, 44.0) | 0.0530 | 12.0 (−21.4, 47.3) | 0.0185 | 11.4 (−22.5, 45.6) | 0.0028 |
| GCS + ankle pump to postoperative baseline | 1.3 (−13.5, 21.9) | 0.3310 | −4.2 (−20.9, 25.2) | 0.5238 | −2.1 (−18.3, 23.1) | 0.2728 |
| GCS + ankle pump to GCS | −1.1 (−10.0, 10.4) | 0.8788 | −0.0 (−12.6, 17.0) | 0.3564 | −0.5 (−11.1, 14.7) | 0.5455 |
| Trough velocity | ||||||
| postoperative to preoperative baseline | 25.1 (−15.3, 100.0) | 0.0002 | 47.0 (−31.8, 174.2) | <.0001 | 34.6 (−24.0, 165.0) | <.0001 |
| GCS to preoperative baseline | 32.2 (−13.3, 158.9) | <.0001 | 59.3 (−8.5, 207.7) | <.0001 | 42.4 (−9.6, 185.1) | <.0001 |
| GCS to postoperative baseline | −1.5 (−25.1, 44.2) | 0.6066 | 1.2 (−21.4, 58.6) | 0.0384 | 0.0 (−22.4, 50.9) | 0.0548 |
| GCS + ankle pump to preoperative baseline | 51.1 (−11.1, 155.8) | <.0001 | 70.7 (−3.2, 191.8) | <.0001 | 64.7 (−7.3, 172.5) | <.0001 |
| GCS + ankle pump to postoperative baseline | −2.3 (−27.4, 56.3) | 0.1374 | 14.0 (−24.3, 93.0) | 0.0019 | 9.8 (−25.1, 73.2) | 0.0007 |
| GCS + ankle pump to GCS | −2.4 (−14.3, 35.7) | 0.3977 | 2.9 (−13.7, 27.7) | 0.0915 | 0.4 (−14.1, 27.8) | 0.0709 |
Notes:
P values were estimated by Wilcoxon signed-rank test for the comparisons before and after interventions.
- GCS
-
graduated compression stocking
Discussion
We compared the efficacy of two GCS types with different graduated pressures on velocity and morphology of femoral veins of the healthy legs among patients after knee replacement and no significant difference was observed between the two types of GCS. However, we found significant elevation of TV in femoral veins after GCS + ankle pump, regardless of GCS types, and the surgery itself would impact the velocity and morphology of femoral veins greatly. In addition, we found that GCS with or without ankle pump may be more effective in improving TV of femoral veins in left leg than that in right leg, implying different prevention strategies of DVT should be considered when dealing with different legs.
In the pilot study conducted in 2022, we compared the impact on femoral vein velocity between three types of GCSs (with different pressure graduated) in healthy volunteers. Significant difference on velocity was revealed between two types of GCS (Yang et al., 2023), while the optimal pressure graduated remains unclear in patients after major orthopedics operations, so this study involving patients with knee replacement was designed. Previous study that enrolled patients only assessed the effectiveness of GCS before the surgery, for instance, Smith, Hasty & Scurr (1991) demonstrated that gastrocnemius vein was reduced by 48% during surgical operation in GCS group while increased by 19% in control groups. Few studies focused on the effect of GCS on velocity or morphology of veins, especially under major orthopedics operations.
The prophylaxis of DVT during perioperative period is essential and previous studies reported GCS could significantly reduce the diameter of deep veins of lower limbs among patients awaiting knee replacement (Jiang et al., 2022; Zhuang et al., 2021). Due to multiple factors brought by the surgery, the conditions of patients after major surgery would vary largely. However, few studies monitored the velocity and morphology of femoral veins of the healthy legs among patients after knee replacement as we did. Our study found that diameters of femoral veins were much smaller within 24 h after the surgery than before knee replacement. Possible reasons may include stress condition, activation of sympathetic adrenergic system, medication during surgery and other factors that would cause vessel contraction. Nevertheless, the hypercoagulable state and immobilization within 24 h after knee replacement still led to the high risk of DVT in both healthy and ill limbs. Therefore, a comprehensive physical prophylaxis strategy of DVT, including GCS and ankle pump, is necessary. Thus, we innovatively monitored the post-surgery condition of the femoral vein and verified the efficacy of GCS + ankle pump.
In this study, we found that GCS + ankle pump significantly improved the velocity of femoral veins in the healthy leg, especially the TV. Although previous study suggested that PV of vein was associated with lower rate of VTE (Keiler, Seidel & Wree, 2019), from the pathophysiological perspective, we believed that elevated TV of the deep vein would yield similar or even more benefit than PV on the prevention of DVT. Further investigations are warranted to explore the relationships between PV/TV and the risk of VTE.
Previous studies showed inconsistent result of vein blood velocity under the application of GCS (Smith, Hasty & Scurr, 1991; Jamieson, Calderwood & Greer, 2007; Keiler, Seidel & Wree, 2019; MacLellan & Fletcher, 2007; Stein et al., 2014; Stein et al., 2010; Toya et al., 2016). However, our study found GCS with/without ankle pump yielded more benefit in left leg on velocity of femoral vein than that in right leg. Previous studies on patients found that DVT occurred more frequently in the lower left extremities. Left iliac veins were more likely to suffer from DVT than the right iliac veins. This may be due to May-Thurner Syndrome, in which the local compression by the right iliac artery may lead to an injury of the left iliac vein, causing stasis which can result in thrombosis. This result was consistent with our pilot study that was conducted among health volunteers and provided clues for specific prophylaxis strategy, for example, different interventions for different legs.
Our study had some limitations: Since the study was conducted within 24 h after the surgery, the legs taking knee replacement were covered with elastic bandages and only the healthy legs were available for GCS. Even though, we believed that it could reflect the actual condition of the systemic condition of the whole body after the surgery. Secondly, during the study period, the effect from the surgery may interfere with the efficacy of GCS with or without ankle pump. Because the postoperative baseline was measured half an hour later after the patient returned to the ward, there were many factors which may affect the diameter and the blood velocity by inducing blood vessel contraction, e.g., the lower temperature in the operation room and vasoactive agent. A longer intervention, such as persistent GCS with or without ankle pump for 48 to 72 h after surgery, may highlight its effectiveness. Furthermore, all the participants were elderly and had relatively high BMI, thus a study conducted in younger participants or with lower BMI is required for enhancing the practical application value of this research. Longer follow-up for assessing long-term effects of GCS is also required.
To our knowledge, this is the first study that analyzed the effects of GCS with or without ankle pump on femoral veins among patients after knee replacement. Although the efficacies between different graduated pressures were comparable, we found that GCS improved the haemodynamic and morphological status of the deep vein on lower limbs. Previously, a previous nation-wide survey demonstrated the current situation of VTE prophylaxis of inpatients that among surgical inpatients, the rate of appropriate prophylaxis (including pharmacological and mechanical) was only 11.8% (Zhai et al., 2019); a recent meta-analysis report that the efficacy of GCS among Asian population after knee replacement as chemical prophylaxis and suggested a routine application of GCS after knee replacement (Wong et al., 2022); the combination of pharmacological prophylaxis and GCS can decrease distal DVT in the lower extremity when compare to pharmacological prophylaxis alone (Lin et al., 2016). Therefore, based on evidence that supports the effectiveness of GCS and its advantages of safety considerations, as well as our findings, more proper prophylaxis would be applied thus less VTE events would happen. Therefore, we would recommend an immediate intervention of GCS (with ankle pump, if possible) after surgery.
Conclusion
The efficacies of two GCSs were comparable, and both were effective in improving velocity and morphology of femoral veins of the healthy legs among patients undergoing knee replacement, especially in improving TV of femoral veins for left leg.
Supplemental Information
Raw data
The efficacy of two different GCSs (group A and B).