The relationship of ulnar variance with pathologies detected by magnetic resonance imaging in patients with chronic or subacute wrist pain
- Published
- Accepted
- Received
- Academic Editor
- Richard Dortch
- Subject Areas
- Anatomy and Physiology, Orthopedics, Radiology and Medical Imaging, Sports Injury, Sports Medicine
- Keywords
- Wrist pain, Ulnar variance, Magnetic resonance, Ulnar impingement, Ulnar impaction
- Copyright
- © 2025 Poçan and Karakaş
- Licence
- This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits using, remixing, and building upon the work non-commercially, as long as it is properly attributed. For attribution, the original author(s), title, publication source (PeerJ) and either DOI or URL of the article must be cited.
- Cite this article
- 2025. The relationship of ulnar variance with pathologies detected by magnetic resonance imaging in patients with chronic or subacute wrist pain. PeerJ 13:e18999 https://doi.org/10.7717/peerj.18999
Abstract
Background
This study aims to determine whether ulnar variance (UV) types are associated with chronic or subacute ulnar-side wrist pain using 3 Tesla (T) magnetic resonance imaging (MRI), and to investigate potential relationships between UV, clinical data, and MRI-detected findings.
Methods
This retrospective study included patients who presented with ulnar-side wrist pain for at least one month and underwent 3T MRI between January 2020 and October 2023. All demographic and clinical data, wrist radiography, and MRI images were obtained from computerized records. The patients were classified as having neutral-UV, negative-UV, and positive-UV.
Results
In total, 272 patients were included in the analysis. Mean age was 40.57 ± 13.18 years and 63.60% (n = 173) of the subjects were female. Neutral UV was detected in 147 (54.04%) patients, negative UV in 106 (38.97%), and positive UV in 19 (6.99%). Patients in the negative-UV group were significantly younger than those in the neutral-UV and positive-UV groups (p = 0.013); however, the sex distribution was similar in all groups (p = 0.653). All patients with ulnar impingement were in the negative-UV group, whereas all subjects with ulnar impaction were in the positive-UV group (p < 0.001). Finally, triangular fibrocartilage complex (TFCC) ruptures were significantly more common in the positive-UV group (p = 0.023).
Conclusion
There is a significant relationship between UV changes and ulnar impingement syndrome, ulnar impaction syndrome, and TFCC tears, which can be easily detected by MRI. The previously reported relationships between UV, sex, and other pathologies were not supported by our findings.
INTRODUCTION
Chronic wrist pain is common and can lead to poor health-related quality of life and functional loss (Ferguson et al., 2019). The complex structure of the wrist and the functional relationships of various anatomical structures contributing to the structure of the joint and those in close proximity make it difficult to identify the etiology of wrist pain (Ferguson et al., 2019; Lee & Nakamura, 2020).
Ulnar variance (UV), also known as Hulten variance (Hultén, 1928), refers to the relationship between the articular surfaces of the distal radius and the distal ulna when the forearm is in its neutral position. UV can be neutral (ulnar and radial joint surfaces are in the same plane), negative (proximal protrusion of the ulna), or positive (distal protrusion of the ulna) (Kamble et al., 2022). UV properties determine the force distribution across the wrist joint, and variations may predispose individuals to pathologies that may cause wrist pain (Athikari, Ramanusan & Subash, 2019; Yoshioka et al., 2007).
UV types are determined via posteroanterior X-rays obtained with the forearm in a neutral position (Tomaino, 2000). However, these images do not reveal soft tissue pathologies. Therefore, magnetic resonance imaging (MRI), which has excellent soft-tissue contrast, can be used to evaluate UV-related soft-tissue pathologies. Relationships between UV and various pathologies have been reported, including conditions that affect the carpal cartilage and other structures such as the bones, fibrocartilage, muscles, tendons, and ligaments (Palmer, Glisson & Werner, 1984; Unver et al., 2004; Yoshioka et al., 2007).
The etiology of wrist pain, the role of UV in wrist pain, and the relationship between UV changes and associated soft and bone tissue pathologies have been investigated in many prior studies (Cilengir et al., 2023; D’Hoore et al., 1994; Stahl et al., 2013; Tomaino & Elfar, 2005). However, radiological studies investigating the relationship between UV characteristics and soft tissue pathologies in the wrist are few (Harley et al., 2015; Van der Post et al., 2022; Yoshioka et al., 2007). Additionally, the relationships between UV and age, sex, and joint side (ulnar or radial) remain unclarified (Bonzar et al., 1998; Hollevoet et al., 2000; Jalan, Elhence & Yadav, 2015; Kamble et al., 2022; Nakamura et al., 1991).
This study aims to evaluate pathologies causing chronic or subacute ulnar-side wrist pain using 3 Tesla (T) MRI and to determine whether UV characteristics are associated with soft-tissue pathologies, as well as clinical and demographic factors. By clarifying possible relationships, we hope to enhance diagnostic accuracy, guide management decisions, and improve the quality of life for patients with chronic wrist pain.
Materials and Methods
Study design and ethics
This retrospective study was conducted at the Radiology Department of BHTCLINIC Istanbul Tema Hospital. Ethical approval was obtained from the Istanbul Nişantaşı University Ethics Committee (Decision date: 04.01.2024, decision no: 20240104-187). The procedures used in this study and all its steps adhered to the Declaration of Helsinki and its amendments. Due to the retrospective design, informed consent requirements were waived.
Study population
Patients who presented with ulnar-side wrist pain persisting for at least 1 month and who underwent 3T MRI between January 2020 and April 2024 were included in the study. Patients younger than 18 years of age, those without MRI results or with images that could not be accessed or had suboptimal quality, those without a reliable wrist radiograph taken in the correct position or could not be used to assess UV, and subjects whose wrist pain was traced to traumatic, mechanical, or congenital causes (for example, Madelung deformity/reverse Madelung deformity) were excluded. Additional exclusion criteria included a history of wrist trauma affecting its structure (e.g., Salter-Harris fracture), wrist surgery, osteoarthritis, or bone or soft-tissue tumors involving the wrist.
Data collection
Data on patients’ age, sex, wrist pain, wrist radiography, and MRI images were collected from the computerized database of our hospital. The affected wrist (right or left) and etiological diagnoses of wrist pain provided by orthopedists or rehabilitation specialists were verified by cross-referencing clinical notes, imaging findings, and diagnostic reports in the patient database. Diagnoses were categorized based on established clinical and radiological criteria to ensure consistency and accuracy.
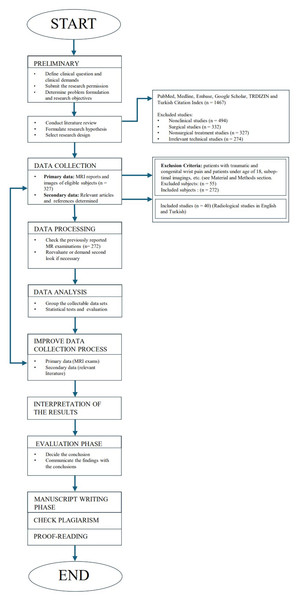
Figure 1 presents the study design, including article and reference selection, subjects included and excluded, and the study process.
Figure 1: The study design including the article and reference selection, subjects included and excluded, and the process of creating the study.
Magnetic resonance imaging protocol
MRI was performed as a routine procedure for patients with chronic wrist pain for whom soft tissue data were deemed necessary for diagnostic purposes. All imaging procedures were performed using a 3T MRI scanner (General Electric Signa Architect, General Electric Healthcare, Waukesha, WI, USA) using a dedicated 16-channel wrist coil (General Electric Healthcare GEM Flex coil 16-L, Pewaukee, WI, USA).
Patients were placed in a feet-first supine position, with the wrist placed in the neutral position alongside the body. The MRI sequences included;
- A coronal T1 fast spin-echo (cor T1 FSE), echo time: 9.3 ms; repetition time: 410 ms; flip angle: 111; slice thickness: three mm; field of view: 120 × 120 mm; matrix: 384 × 384; spatial resolution: 0.31–0.31 mm)
- Coronal short Tau inversion recovery (cor STIR), echo time: 55.1 ms; repetition time: 5,893 ms; flip angle: 111; slice thickness: three mm; field of view: 120 × 120 mm; matrix: 256 × 172; spatial resolution: 0.46–0.69 mm)
- Coronal 3-dimensional Multiple Echo Recombined Gradient Echo (cor 3D MERGE), echo time: 11.6 ms; repetition time: 44 ms; flip angle: 5; slice thickness: two mm; field of view: 120 × 120 mm; matrix: 288 × 256; spatial resolution: 0.41–0.46 mm)
- Axial proton density fat saturated fast spin-echo (ax PD FSE FS), echo time: 25.8 ms; repetition time: 3,211 ms; flip angle: 111; slice thickness: three mm; field of view: 110 × 110 mm; matrix: 320 × 256; spatial resolution: 0.37–0.46 mm)
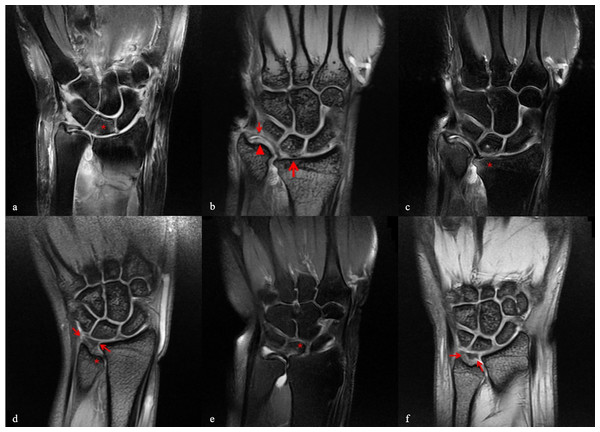
- Axial T1 fast spin-echo (ax T1 FSE), echo time: 9.7 ms; repetition time: 619 ms; flip angle: 90; slice thickness: three mm; field of view: 110 × 110 mm; matrix: 384 × 320; spatial resolution: 0.31–0.37 mm), sagittal proton density fat saturated ((sag PD FS), echo time: 32.4 ms; repetition time: 3,823 ms; flip angle: 111; slice thickness: three mm; field of view: 120 × 120 mm; matrix: 320 × 240; spatial resolution: 0.37–0.5 mm) (Fig. 2).
Figure 2: Case examples.
(A) A case with positive ulnar variance. In coronal PD FSAT section, medullary edema in the lunate bone was evaluated as impaction (asterix); (B) and (C) TFCC (thin arrow) and ulnar articular cartilage damages (triangle) accompanied by positive ulnar variance (asterix and thick arrow) in Coronal MERGE and Coronal PD FSAT sections of the same patient; (D) In the Coronal MERGE section of the patient with obvious negative ulnar variance, despite the ulnar impingement (asterix), TFCC is observed to have preserved its normal triangular form and signal intensity (thin arrow); (E) In the case with negative ulnar variance, TFCC deformation and medullary edema in the lunate bone (asterix) are observed in the Coronal PD FSAT section; (F) In the case with negative ulnar variance, TFCC partial tear (thin arrow) and ulnar impingement (thick arrow) were visualized in the Coronal MERGE section.The image reports were assessed by two radiologists with 10 years of experience in wrist MRI evaluation. The parameters investigated included ulnar impingement and/or impaction syndrome, ganglion cysts (presence and type), tendon pathologies (e.g., tendinopathy, tenosynovitis, sprain, degeneration), bone pathologies (e.g., edema, necrosis, cysts, impaction), muscle pathologies (e.g., rupture, strain, degeneration), triangular fibrocartilage complex (TFCC) pathologies, ligament pathologies, and other masses (e.g., tumors, cysts, neuromas, lipomas, thromboses). Pathologies were classified based on a combination of imaging characteristics and clinical findings. The diagnoses of ulnar impingement and impaction syndromes were made based on MRI findings, which included the assessment of specific structural changes observed in the ulnar-sided wrist. These changes included altered alignment, degeneration of cartilage, and any signs of impaction or abnormal contact between the ulnar bone and adjacent structures. MRI sequences, particularly those focusing on soft tissue and bone integrity, were utilized to evaluate these changes. The criteria for diagnosis followed those established in previous studies (Cerezal et al., 2002; Sattar, Weerakkody & Feger, 2024), while other pathologies such as ganglion cysts, tendon abnormalities, and bone pathologies were assessed using standardized radiological descriptions. For ligamentous and TFCC injuries, the classification was guided by severity (e.g., sprain, partial rupture, complete rupture) and accompanying degeneration or deformation, as observed on MRI. Radiologists used a predefined checklist to ensure consistency in evaluating all parameters.
UV examination
Wrist radiographs were obtained in the neutral position using a General Electric Healthcare Optima XR646 digital X-ray device in the posteroanterior view, with the arm abducted and the elbow flexed at 90°. The source-to-patient distance was 100 cm, with a tube current of 80–100 mA (adjusted for fine focus), a voltage of 60–65 kV, and an exposure time of 20 ms. The irradiated area was 24 × 30 cm2 on a digital flat-panel detector, and the beam incidence was set at a 90° angle to the surface.
UV evaluation was performed using the perpendicular method, measuring the distance between the cortical edges of the distal radius and ulna. A distance of > one mm proximal to the ulna was defined as showing negative UV, while > one mm distal distance was indicative of positive UV (Sayit et al., 2018). Patients were classified into neutral-UV, negative-UV, and positive-UV groups.
Statistical analysis
A two-tailed p-value of less than 0.05 was considered statistically significant. Statistical analyses were conducted using IBM SPSS Statistics for Windows (version 25.0; IBM Corp., Armonk, NY, USA). Assessment of normal distribution for continuous variables involved the examination of histograms and Q-Q plots. Descriptive statistics are reported as mean ± standard deviation for normally distributed continuous variables and as frequency (percentage) for categorical variables. One-way analysis of variance (ANOVA) was used for the comparisons of normally distributed continuous variables, while categorical variables were analyzed using either the chi-square test or the Fisher–Freeman–Halton test. Pairwise comparisons were performed using the Bonferroni correction.
Results
In total, 327 patients were investigated for eligibility. Fifty-three patients were excluded because they had traumatic wrist pain (e.g., fractures). Two patients were excluded because they were younger than 18 years of age. In total, 272 patients were included in the analysis. Overall mean age was 40.57 ± 13.18 years and 63.60% (n = 173) of the patients were females. Wrist pain was on the right wrist in 141 (51.84%) patients and on the left wrist in 131 (48.16%) patients. Radiographic images revealed that neutral UV was present in 147 (54.04%) patients, negative UV in 106 (38.97%), and positive UV in 19 (6.99%). The demographic, clinical, and radiological data of the patients are presented in Table 1.
| Age, years | 40.57 ± 13.18 |
| Sex | |
| Male | 99 (36.40%) |
| Female | 173 (63.60%) |
| Side | |
| Right | 141 (51.84%) |
| Left | 131 (48.16%) |
| Ulnar variance | |
| Neutral | 147 (54.04%) |
| Negative | 106 (38.97%) |
| Positive | 19 (6.99%) |
| Syndrome | 16 (5.88%) |
| Ulnar impingement | 11 (4.04%) |
| Ulnar impaction | 4 (1.47%) |
| Both | 1 (0.37%) |
| Ganglion cyst | 79 (29.04%) |
| Tendon pathology(1) | 45 (16.54%) |
| Tendinopathy | 28 (10.29%) |
| De Quervain’s tenosynovitis | 14 (5.15%) |
| Other tenosynovitis | 2 (0.74%) |
| Sprain | 4 (1.47%) |
| Degeneration | 2 (0.74%) |
| Bone pathology(1) | 93 (34.19%) |
| Edema | 39 (14.34%) |
| Kienböck’s disease | 10 (3.68%) |
| Other necrosis | 1 (0.37%) |
| Cyst | 54 (19.85%) |
| Impaction | 1 (0.37%) |
| Muscle pathology | 6 (2.21%) |
| Rupture | 3 (1.10%) |
| Strain | 2 (0.74%) |
| Degeneration | 1 (0.37%) |
| TFCC pathology(1) | 64 (23.53%) |
| Rupture | 47 (17.28%) |
| Sprain | 4 (1.47%) |
| Degeneration | 2 (0.74%) |
| Deformation | 12 (4.41%) |
| Cyst | 1 (0.37%) |
| Other ligament pathology | 5 (1.84%) |
| Rupture | 4 (1.47%) |
| Degeneration | 1 (0.37%) |
| Other pathological mass | 6 (2.21%) |
| Giant cell tumor | 1 (0.37%) |
| Neuroma | 1 (0.37%) |
| Synovial cyst | 1 (0.37%) |
| Enchondroma | 1 (0.37%) |
| Lipoma | 1 (0.37%) |
| Varix thrombosis | 1 (0.37%) |
Notes:
Descriptive statistics were presented by using mean ± standard deviation for continuous variables and frequency (percentage) for categorical variables.
(1) Patients may have more than one of the following.
- TFCC
-
Triangular fibrocartilage complex
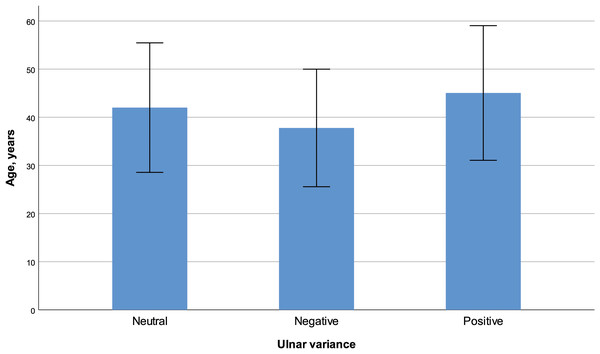
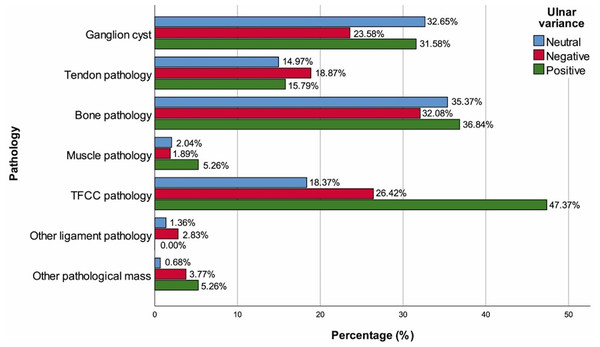
The mean age of the negative-UV group was significantly lower than that of both the neutral-UV and positive-UV groups (p = 0.013, Fig. 3). There was no significant difference in sex distribution between the groups (p = 0.653). Patients with right wrist pain had significantly higher frequencies of both negative-UV and positive-UV when compared to patients with left wrist pain (p = 0.024). All patients with ulnar impingement were in the negative-UV group and all patients with ulnar impaction were in the positive-UV group (p < 0.001 for both). TFCC pathologies were more common in the Positive-UV group (p = 0.013), with a significantly higher frequency of TFCC rupture (p = 0.023). The groups demonstrated similar characteristics in terms of other MRI findings (Table 2, Fig. 4).
Figure 3: Age (mean ± standard deviation) with regard to ulnar variance.
| Ulnar variance | ||||
|---|---|---|---|---|
| Neutral (n = 147) | Negative (n = 106) | Positive (n = 19) | p | |
| Age, years | 42.01 ± 13.45 | 37.78 ± 12.21* | 45.05 ± 13.99# | 0.013a |
| Sex | ||||
| Male | 51 (34.69%) | 42 (39.62%) | 6 (31.58%) | 0.653b |
| Female | 96 (65.31%) | 64 (60.38%) | 13 (68.42%) | |
| Side | ||||
| Right | 65 (44.22%) | 64 (60.38%)* | 12 (63.16%)* | 0.024b |
| Left | 82 (55.78%) | 42 (39.62%) | 7 (36.84%) | |
| Syndrome | 0 (0.00%) | 11 (10.38%)* | 5 (26.32%)* | <0.001b |
| Ulnar impingement | 0 (0.00%) | 11 (10.38%)* | 0 (0.00%)# | <0.001c |
| Ulnar impaction | 0 (0.00%) | 0 (0.00%) | 4 (21.05%)*# | |
| Both | 0 (0.00%) | 0 (0.00%) | 1 (5.26%) | |
| Ganglion cyst | 48 (32.65%) | 25 (23.58%) | 6 (31.58%) | 0.283b |
| Tendon pathology(1) | 22 (14.97%) | 20 (18.87%) | 3 (15.79%) | 0.709b |
| Tendinopathy | 14 (9.52%) | 14 (13.21%) | 0 (0.00%) | 0.197b |
| De Quervain’s tenosynovitis | 7 (4.76%) | 5 (4.72%) | 2 (10.53%) | 0.546b |
| Other tenosynovitis | 1 (0.68%) | 1 (0.94%) | 0 (0.00%) | 1.000c |
| Sprain | 3 (2.04%) | 0 (0.00%) | 1 (5.26%) | 0.108c |
| Degeneration | 2 (1.36%) | 0 (0.00%) | 0 (0.00%) | 0.577c |
| Bone pathology(1) | 52 (35.37%) | 34 (32.08%) | 7 (36.84%) | 0.835b |
| Edema | 23 (15.65%) | 14 (13.21%) | 2 (10.53%) | 0.763b |
| Kienböck’s disease | 4 (2.72%) | 4 (3.77%) | 2 (10.53%) | 0.194c |
| Other necrosis | 1 (0.68%) | 0 (0.00%) | 0 (0.00%) | 1.000c |
| Cyst | 33 (22.45%) | 18 (16.98%) | 3 (15.79%) | 0.504b |
| Impaction | 1 (0.68%) | 0 (0.00%) | 0 (0.00%) | 1.000c |
| Muscle pathology | 3 (2.04%) | 2 (1.89%) | 1 (5.26%) | 0.510c |
| Rupture | 1 (0.68%) | 2 (1.89%) | 0 (0.00%) | 0.657c |
| Strain | 1 (0.68%) | 0 (0.00%) | 1 (5.26%) | 0.135c |
| Degeneration | 1 (0.68%) | 0 (0.00%) | 0 (0.00%) | 1.000c |
| TFCC pathology(1) | 27 (18.37%) | 28 (26.42%) | 9 (47.37%)* | 0.013b |
| Rupture | 19 (12.93%) | 21 (19.81%) | 7 (36.84%)* | 0.023b |
| Sprain | 1 (0.68%) | 2 (1.89%) | 1 (5.26%) | 0.178c |
| Degeneration | 0 (0.00%) | 1 (0.94%) | 1 (5.26%) | 0.059c |
| Deformation | 7 (4.76%) | 4 (3.77%) | 1 (5.26%) | 0.813c |
| Cyst | 0 (0.00%) | 1 (0.94%) | 0 (0.00%) | 0.460c |
| Other ligament pathology | 2 (1.36%) | 3 (2.83%) | 0 (0.00%) | 0.759c |
| Rupture | 2 (1.36%) | 2 (1.89%) | 0 (0.00%) | 1.000c |
| Degeneration | 0 (0.00%) | 1 (0.94%) | 0 (0.00%) | 0.460c |
| Other pathological mass | 1 (0.68%) | 4 (3.77%) | 1 (5.26%) | 0.134c |
| Giant cell tumor | 1 (0.68%) | 0 (0.00%) | 0 (0.00%) | 1.000c |
| Neuroma | 0 (0.00%) | 1 (0.94%) | 0 (0.00%) | 0.460c |
| Synovial cyst | 0 (0.00%) | 0 (0.00%) | 1 (5.26%) | 0.070c |
| Enchondroma | 0 (0.00%) | 1 (0.94%) | 0 (0.00%) | 0.460c |
| Lipoma | 0 (0.00%) | 1 (0.94%) | 0 (0.00%) | 0.460c |
| Varix thrombosis | 0 (0.00%) | 1 (0.94%) | 0 (0.00%) | 0.460c |
Notes:
Descriptive statistics were presented by using mean ± standard deviation for continuous variables and frequency (percentage) for categorical variables.
(1) Patients may have more than one of the following.
a: One-way analysis of variance, b: Chi-square test, c: Fisher-Freeman-Halton test.
- TFCC
-
Triangular fibrocartilage complex
Figure 4: Percentage of radiological findings with regard to ulnar variance.
Discussion
Chronic wrist pain is a common clinical condition. For optimal wrist movement, the distal joint surface of the radius and ulna must be at the same level (Jalan, Elhence & Yadav, 2015). Even small differences in this joint feature can change load distribution, causing various pain syndromes. It has been demonstrated that UV is an important parameter in evaluating load distribution and plays a major role in the etiopathogenesis of wrist pain (Jalan, Elhence & Yadav, 2015; Sayit et al., 2018). In this study, we investigated the relationship between UV and wrist joint pathologies detected using 3T MRI, and other demographic and clinical variables. The current retrospective cohort revealed that in patients with chronic or subacute wrist pain, the frequency of neutral UV was 54.04%, negative UV was 38.97%, and positive UV was 6.99%, which is consistent with previous studies (Athikari, Ramanusan & Subash, 2019; Kamble et al., 2022; Waris et al., 2023). The incidence of negative UV was elevated among younger patients, whereas older patients were more likely to have positive UV results. All patients with ulnar impingement syndrome had negative UV, while all patients with ulnar impaction syndrome had positive UV. Additionally, TFCC ruptures were significantly more prevalent in patients with positive UV.
UV has been associated with wrist pathologies (Cilengir et al., 2023) and sports/activities (Scigliano et al., 2024), and a number of biochemical and biomechanical factors can underlie the macroscopic impact of UV on soft tissue changes, including inflammation, oxidative stress, and anthropomorphic characteristics (Liu et al., 2022; Samadi et al., 2021; Sophia Fox, Bedi & Rodeo, 2009). In terms of clinical data, various radiological and clinical studies have investigated the relationships between UV features and other pathologies of the wrist joint (Harley et al., 2015; Iordache et al., 2012; Van der Post et al., 2022; Yoshioka et al., 2007). However, the relationship between UV changes and MRI-detectable pathologies in patients with chronic wrist pain remains controversial. The relationship of ulnar impaction syndrome with positive UV (Darlis et al., 2005; Tomaino & Elfar, 2005) and the relationship of ulnar impingement syndrome with negative UV (Jung et al., 2001; Stahl et al., 2013) has already been shown in previous studies and is generally accepted. Evidence also suggests a causal relationship between negative UV and Kienböck’s disease, but this has not been corroborated by other studies (D’Hoore et al., 1994; Sayit et al., 2018; Stahl et al., 2013). Cilengir et al. (2023) showed a significant relationship between UV and the presence of pisotriquetral joint subluxation, an important cause of ulnar-sided wrist pain. Pisotriquetral joint subluxation is less common in patients with neutral or negative UV than in those with positive UV. There also exist some isolated studies which report other effects of UV. For instance, Cha, Shin & Song (2019) reported that positive UV had an important role in the development of carpal tunnel syndrome. The current study confirmed the associations between negative UV and ulnar impingement syndrome as well as the relationship between positive UV and ulnar impaction syndrome. However, other bone (including Kienböck’s disease), muscle, tendon, and ligament pathologies investigated in the study, other than TFCC rupture, were not found to be associated with UV categories.
The TFCC is a fibrocartilage-ligament complex extending in the ulna and ulnar carpus area that originates from the radius and attaches to the distal ulna, contributing to the structure of the wrist joint (Yoshioka et al., 2007). The TFCC facilitates the integrity of the distal ulna and ulnar carpus, and provides stability to the distal radioulnar joint. Owing to these anatomic and functional features, there may be a conceivable relationship between UV characteristics and TFCC injuries, which has been demonstrated with convincing evidence alongside the impact of UV on ulnar impaction syndrome (Cerezal et al., 2002; Imaeda et al., 1996; Mellado et al., 2003). As a consequence of positive UV, there appears to be a substantial increase in the compression load from the center of the TFCC disc to the head of the ulna. Conversely, a negative ulnar variation may result in increased tension within the TFCC (Cerezal et al., 2002; Yoshioka et al., 2007). Chronic impaction between the head of the ulna, ulnar carpus, and TFCC due to positive UV results in ulnar impaction syndrome, which is one of the most common causes of ulnar-side wrist pain (Cerezal et al., 2002). The current study showed that positive UV was more frequently associated with TFCC rupture compared to neutral and negative UV, though the statistical power to definitively confirm this association is limited.
Yoshioka et al. (2007) concluded that high-resolution MRI with a microscopy coil can be a helpful instrument for the assessment of the ulnar-side structures of the wrist, notably the TFCC and cartilage related to UV. Indeed, a moderate negative correlation between TFCC thickness and UV exposure has been revealed using high-resolution images (Van der Post et al., 2022). Ryoo et al. (2023) showed that UV increased after TFCC foveal tear and positive UV decreased after arthroscopic transosseous TFCC foveal repair. Similarly, a number of authors have described a negative correlation between TFCC thickness and UV exposure (Harley et al., 2015; Iordache et al., 2012; Yoshioka et al., 2007). Unglaub et al. (2010) showed that the density of cells positive for proliferating cell nuclear antigen in TFCC was higher in patients with negative or neutral UV than in those with positive UV. Another study reported that the number of apoptotic and necrotic cells in the TFCCs of patients with degenerative TFCC ruptures was significantly higher in patients with positive UV compared to those with neutral UV (Unglaub et al., 2008). Van der Post et al. (2022) claimed that such results may explain why patients with negative UV have a thicker TFCC in relation to higher proliferation. Our study supports these results and hypotheses. We believe that it is crucial to understand the relationship between UV and ulnar-sided structures of the wrist, such as the TFCC, lunate and ulnar head cartilage (and others). It is evident that 3T MRI offers an excellent imaging opportunity to evaluate these structures and pathologies, indicating the need for further studies utilizing high-resolution imaging in these cases.
In this study, in addition to radiological findings, the relationships between age, sex, side of wrist pain and UV were also investigated. We showed that negative UV may be associated with younger age, and positive UV may be associated with older age compared to negative UV. Both positive and negative UV were significantly more common in those with right-sided wrist pain; however, it is reasonable to associate this finding with hand dominance and the impact of this on wrist pathology. There were no significant differences between the sexes in terms of UV. The association between UV and age, sex, and side remains controversial, and our findings indicate that such variations may not be generalizable to the general population. Conflicting results are common in the literature, but some notable evidence deserves mention. While some studies report no relationship between age and UV (Jalan, Elhence & Yadav, 2015; Namazi & Khaje, 2015; Sayit et al., 2018), others claim that UV distance measures increase with age (Bonzar et al., 1998; Kamble et al., 2022; Nakamura et al., 1991; Öztürk et al., 2021). This could be associated with the utilization of different measurement methods, as revealed by the significant variations among different UV assessment methods (Öztürk et al., 2021). Studies investigating the relationship between sex and UV have also presented distinct results (Bonzar et al., 1998; Jalan, Elhence & Yadav, 2015; Kamble et al., 2022; Nakamura et al., 1991; Namazi & Khaje, 2015; Öztürk et al., 2021; Sayit et al., 2018), which shows the need for large-scale and preferably population-based studies to understand whether UV features are affected by sex. Although more studies have reported that UV does not differ between the right and left extremities (Kamble et al., 2022; Sayit et al., 2018; Waris et al., 2023), it has also been reported that increased UV is more pronounced on the right side (Hollevoet et al., 2000). Possible reasons for these indistinct results may be the impact of hand dominance and anthropometric features (load and load-bearing differences), radiological measurement tools and techniques used for UV assessment, and the position of the shoulder, arm, and wrist when imaging was performed. It is also evident that racial differences between the selected study populations could contribute to the differing data and interpretations. Furthermore, some researchers have claimed that X-rays are less predictive of negative UV than MRI and computed tomography (Kawanishi et al., 2014). As previously mentioned, the measured methodologies also impact the data. Various methods have been described to measure UV. The most popular methods are the project-a-line technique, the circular method, and the perpendicular method (Sayit et al., 2018). Although all three methods have been shown to be reliable, the perpendicular method is recommended because of its better (lower) intra- and interobserver variability. The UV measurements in the present study were performed using the perpendicular method to increase the reliability of the results. However, the relationship between UV and age, sex, and side appears to be a controversial issue that requires further research.
While this study has demonstrated notable associations between UV and specific wrist conditions, it is crucial to emphasize that these relationships do not imply causation. Further prospective studies, including longitudinal and experimental designs, are necessary to better understand the underlying mechanisms and to establish whether UV directly contributes to the development of these conditions. Future research should also consider controlling for potential confounders such as hand dominance, activity levels, and other biomechanical factors that may influence UV. The current study provides important evidence regarding the role of UV in chronic or subacute wrist pain which can be a basis for further investigations that should consider the fact that these relationships do not imply causation.
This was a retrospective study conducted at a single center, which limits the investigation of new data and generalizability of the results. Since debates about UV definitions and thresholds are still ongoing, in this study, we preferred to divide the patients into positive, negative, and neutral UV rather than providing numerical UV values. This may be seen as a limitation by some, but this approach allows for categorization, which serves the purpose of the present study. Since we focused on radiological data, clinical severity indicators such as detailed physical examination findings, symptom scores of the patients, and dominant hand information could not be included. The fact that the number of patients with positive UV was lower, in line with previously reported general population data, may have reduced the power of the statistical comparisons in this respect. However, it is evident that the group sizes are respectable in relation to the group sizes reported in the majority of the literature on this topic. The study population comprised patients with chronic or subacute wrist pain. This makes it difficult to establish a causal relationship between UV and other wrist pathologies. Despite these limitations, this study provides important data regarding the relationship between MRI-detected pathologies and UV in patients with chronic or subacute wrist pain and contributes to the literature by addressing the lack of comprehensive data on this subject.
CONCLUSIONS
Among patients experiencing chronic or subacute wrist pain, younger individuals were more likely to have negative UV, whereas older patients demonstrated a higher frequency of positive UV. Notably, negative UV was strongly associated with ulnar impingement syndrome, while positive UV was associated with ulnar impaction syndrome. A significant link was identified between positive UV and TFCC ruptures. Despite ongoing debates regarding the correlation of UV changes with age, sex, and lateralization in individuals with chronic wrist pain, our results demonstrate notable relationships between UV variations and MRI-detectable findings, such as ulnar impingement syndrome, ulnar impaction syndrome, and TFCC tear.
Supplemental Information
Dataset
Data of the MR examination of the affected location, time of examination, patient age and gender, pathologies which are primarily investigated, type of ulnar variance.