Clinical outcomes of arthroscopic suture fixation combined with loop plate vs. posterior approach open reduction and cannulated screw fixation for treating tibial avulsion fractures of the posterior cruciate ligament: a retrospective study
- Published
- Accepted
- Received
- Academic Editor
- Yoshinori Marunaka
- Subject Areas
- Anatomy and Physiology, Orthopedics, Rheumatology, Surgery and Surgical Specialties
- Keywords
- Adolescent, Arthroscopic suture fixation, Knee instability, Open reduction and internal fixation, Posterior cruciate ligament, Tibial avulsion fracture
- Copyright
- © 2024 Zhang and Guo
- Licence
- This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits using, remixing, and building upon the work non-commercially, as long as it is properly attributed. For attribution, the original author(s), title, publication source (PeerJ) and either DOI or URL of the article must be cited.
- Cite this article
- 2024. Clinical outcomes of arthroscopic suture fixation combined with loop plate vs. posterior approach open reduction and cannulated screw fixation for treating tibial avulsion fractures of the posterior cruciate ligament: a retrospective study. PeerJ 12:e18532 https://doi.org/10.7717/peerj.18532
Abstract
Background
Comparison of the efficacy of arthroscopic suture fixation combined with loop plate vs. the posterior approach involving open reduction and intramedullary nail fixation in treating posterior cruciate ligament tibial avulsion fractures (PCLTAFs).
Methods
A retrospective analysis was conducted on the clinical data of patients diagnosed with PCLTAF who were admitted to Northern Jiangsu People’s Hospital between June 2019 and March 2022. Based on distinct surgical procedures, the patients were categorized into two groups: arthroscopic group (33 cases), involving a single bone tunnel, high-strength suture, loop plate, and anchor screw fixed under arthroscopy, and open reduction and internal fixation (ORIF) group (13 cases), involving a modified posterior medial approach and fixation using 1–2 cannulated screws. Key parameters, including surgical duration, postoperative fracture alignment, fracture-healing duration, range of motion changes, postoperative Lysholm scores, and VAS scores were documented and compared between the two groups.
Results
The study cohort comprised 46 patients, with 28 males and 18 females, and the median age was 29 years old (range: 15–69). There were no significant differences in the baseline characteristics, including knee Lysholm scores, between the two groups. The arthroscopic group exhibited significant improvement in all eight Lysholm score indicators (all P < 0.001). The total Lysholm score also exhibited significant improvement before and after surgery in both groups (P < 0.001). Following surgery, the arthroscopic group demonstrated improvements in all indicators, but had a slightly longer operating time compared to the ORIF group. No significant differences were observed in the Lysholm scores for the knee joint between the two patient groups before and after surgery (P > 0.05).
Conclusions
Arthroscopic suture fixation in conjunction with looped plate binding can significantly improve knee function and clinical effect for patients in the treatment of PCLTAF, promotingearly postoperative functional recovery of patients.
Introduction
The posterior cruciate ligament (PCL) constitutes a vital element of the knee joint’s ligamentous structure. It serves to inhibit posterior displacement of the tibia, prevent excessive knee hyperextension, and safeguard rotation of the knee joint (Liu et al., 2021; D’Ambrosi, Halle & Hardy, 2023). Furthermore, the PCL acts as a primary stabilizing factor and serves as the axis of rotation, making it crucial for maintaining the static stability of the knee joint. It can bear a huge load in the posterior direction (Yang et al., 2024). Tibial avulsion fractures involving posterior cruciate ligament insertion, a distinct subset of PCL injuries, exhibit a relatively low incidence in clinical scenarios. These fractures usually result from a forceful impact directly to the tibia during knee joint flexion, leading to a posterior shift or significant hyperextension of the knee joint (Gopinatth et al., 2023). The clinical presentation of posterior cruciate ligament tibial avulsion fractures (PCLTAFs) shares similarities with PCL ruptures and often leads to post-injury knee instability. Neglected cases of displaced PCL insertion avulsion fractures can compromise the knee joint’s normal mechanical function, potentially culminating in secondary osteoarthritis. In severe instances, these fractures can lead to concomitant meniscal and osteochondral injuries (Katsman et al., 2018; Khalifa et al., 2021).
Currently, the prevalent surgical approaches for addressing PCL insertion avulsion fractures encompass arthroscopic reduction fixation and posterior open reduction and internal fixation (ORIF), with both aimed at achieving improved bone healing (Sundararajan et al., 2021b). Arthroscopic reduction and fixation is a minimally invasive technique using high-strength sutures and annular plates. It has the benefits that it minimizes the risk of damage to the surrounding tissues and allows for early rehabilitation (Zhu et al., 2017). The ORIF method, on the other hand, uses a modified posteromedial approach for fixation with a cannulated screw. Although widely used in clinical practice, it has some limitations, such as the risk of nerve and vascular injury and excessive soft tissue dissection (Khatri et al., 2015; Hooper et al., 2018). The benefits of arthroscopy are widely recognized; nonetheless, challenges persist, including rigorous demands for accurate reduction and fixation, along with a steep learning curve. Additionally, arthroscopic systems can be costly and can encounter difficulties in achieving precise reduction in cases of severely displaced comminuted fractures (Sundararajan et al., 2021b). Also, PCL reconstruction under arthroscopy has a higher risk of complications compared to other arthroscopic knee surgeries, including neurovascular injuries, compartment syndrome, persistent posterior laxity, loss of motion, osteonecrosis, and heterotopic ossification (James, Taber & Marx, 2021). Some studies have also reported a heightened occurrence of joint fibrosis subsequent to arthroscopy compared with open surgery (Hooper et al., 2018). A biomechanical investigation demonstrated that there was no notable disparity between open and arthroscopic fixation techniques (Song, Nha & Lee, 2018).
There is consensus regarding the necessity of surgical intervention for displaced PCLTAFs, but not the preferred method. Though ORIF is a standard technique, it is more suited for managing larger bone fragments than smaller or comminuted fractures (Kan et al., 2020; Xiong et al., 2023). Conversely, the arthroscopic technique offers the potential for achieving anatomical fracture reduction, dependable healing, and preventing subsequent knee joint instability (Zhu et al., 2017). Nevertheless, numerous arthroscopic fixation methods for PCLTAFs are available, each differing in terms of surgical complexity and efficacy. This study aimed to compare the pain (Visual Analog Scale, VAS) and joint mobility (Lysholm Knee Score) between arthroscopic fixation and ORIF in a cohort of 46 PCLTAF patients, with the goal of furnishing empirical evidence to determine the superior clinical treatment approach for this specific fracture type.
Materials and Methods
Study design and participants
This retrospective study involved the analysis of clinical data from 46 patients with PCLTAF who were admitted to Northern Jiangsu People’s Hospital between June 2019 and March 2022. The patients were categorized into two distinct groups: an arthroscopic group, comprising 33 cases, who had underwent treatment involving a single bone tunnel, high-strength suture, loop plate, and anchor screw fixed under arthroscopy; and an ORIF group, comprising 13 cases, who had underwent treatment involving a modified posterior medial approach to the knee joint and fixation using 1–2 cannulated screws. Surgical procedures for both groups were performed by the same surgical team. The study was granted approval by the Ethics Committee of Northern Jiangsu People’s Hospital (Protocol No. 2021ky182-1), and written informed consent was obtained from all the patients and their respective families.
The inclusion criteria comprised the following: (1) Preoperative X-ray, CT, and MRI examinations confirming intact PCL parenchyma and the presence of PCLTAF; (2) Meyer–McKeever types II, III, or IV fractures (Meyers & McKeever, 1970); (3) fresh fractures occurring within 3 weeks of the injury; (4) positive posterior knee drawer test; (5) post-surgery follow-up duration of ≥12 months with comprehensive clinical data. The exclusion criteria encompassed the following: (1) open injuries or injuries associated with skin and soft tissue infections, or significant vascular and nerve damage; (2) concomitant tibial plateau fractures; (3) injuries involving the anterior cruciate ligament, as well as internal and external collateral ligament injuries; (4) presence of associated posterior corner injuries; (5) presence of chronic pain, restricted mobility, or osteoarthritis prior to surgery.
Procedures
In the arthroscopy procedures performed at our hospital, the patients were positioned supine, administered routine anesthesia, and subjected to tourniquet hemostasis. Initial exploration involved the anterior internal and external knee arthroscopy approaches to assess intra-articular injuries and determine the appropriate treatment. Subsequently, both high and low posterior medial approaches were established, with the high-level approach facilitating observation and the low-level approach serving as an instrumental conduit. The posterior intercondylar fossa was accessed to expose the posterior cruciate ligament, from which blood clots and soft tissue around the fracture were removed. The posterior cruciate ligament was anchored at its tibial attachment site using a high-strength suture, and employing a suture hook through the anterior approach. Subsequently, the high-strength suture was threaded through a loop plate. Furthermore, a bone tunnel was fashioned along the posterior cruciate ligament reconstruction locator within the intercondylar notch. Employing a 4.5 mm hollow drill guided by a Kirschner wire, a solitary bone tunnel was established, extending from the anterior tibia to the fracture fragment. Through this tunnel, the guidewire was inserted from anterior to posterior. The high-strength suture threaded through the loop plate was then extracted from the bone tunnel and tensioned to compress the fracture fragment. A singular anchor screw was positioned within the anterior knee tunnel, following which the high-strength suture was maximally tensioned and secured to the anchor screw.
In the ORIF procedures performed at our hospital, the patients were positioned prone, administered routine anesthesia, and underwent tourniquet hemostasis. Utilizing a modified medial approach with a 4 cm straight incision to the posterior aspect of the knee joint, the fractured area within the gap between the semimembranosus muscle and the medial head of the gastrocnemius muscle was unveiled, thereby exposing the avulsed fragment of the tibial intercondylar eminence. Subsequent steps included the removal of tissues embedded at the fracture site, followed by the reduction of the fracture fragment and the introduction of 1–2 guide needles for cannulated screws. Upon achieving satisfactory positioning within the C-arm machine, 1–2 cannulated screws measuring 3.5 mm were employed to achieve compression fixation, the choice being determined by the size of the fractured fragment. Confirmation of the avulsed fragment’s alignment was undertaken through utilization of the C-arm machine following fixation. This was followed by layered closure of the incision.
Postoperative rehabilitation exercises
Both patient groups engaged in knee function exercises guided by rehabilitation specialists. Following the surgery, adjustable hinged supports were affixed to the knee joint. In the initial 4 weeks, the knee joint was stabilized at a 0° angle, with straight leg raises employed for quadriceps training, complemented by ankle flexion and extension exercises. Passive knee flexion exercises commenced 3 days post-surgery, progressively reaching 90° within 4 weeks and 120° within 6 weeks. For the initial 6 weeks, the affected limb was not subjected to weight-bearing, transitioning to partial weight-bearing from 6 to 8 weeks. Subsequently, full-weight-bearing was allowed after 8 weeks, while the knee joint immobilizer remained in place for 12 weeks post-surgery. Complete restoration of the normal movement should be attained by 6-month post-operation.
Assessments
The operation time, preoperative, and postoperative Lysholmscores, and VAS scores were recorded for all patients. Here, we compared the data for both groups. Given that a tourniquet was employed during surgery for both groups, comparison of blood loss held no relevance, and so this is not considered further in this article. For assessing postoperative fracture reduction, routine follow-up occurred at the outpatient department for a duration of 1 year for all the patients. This involved obtaining anteroposterior and lateral knee joint X-rays at intervals of 1, 3, and 12 months post-operation. These images were utilized to assess fracture reduction and healing across both groups. The evaluation of the knee joint functional activity involved the use of the Lysholm score to gauge the recovery of knee joint functionality within both groups. This Lysholm knee scoring system encompassed eight dimensions: limping, assistive device requirement, joint stability, joint restraining, joint swelling, capacity to ascend stairs, capacity to squat, and joint pain.
To objectively evaluate the patient’s pain level, the visual analog score (VAS) is generally employed. The VAS was obtained by taking a 10-cm-long straight line, with one end indicating no pain (0 points) and the other indicating the most severe pain (10 points), and asking the patients to mark a point on the straight line based on their current level of pain. VAS scores were recorded before surgery, and on the 1st, 3rd, 7th, and 30th day after surgery.
Bias and potential confounding factors
Selection bias: Due to the retrospective design of this study, there may be a risk of selection bias. Specifically, the selection and grouping of patients were not random, which could result in an incomplete balance of the baseline characteristics between the two groups. To minimize this bias, we recorded and compared the baseline characteristics of the patients in detail to ensure there were no significant differences between the two groups.
Information bias: There may be information bias during the data collection process. Although we strived to ensure the accuracy and completeness of data, retrospective data collection may be affected by incomplete or inconsistent records. For this reason, we performed strict auditing and verification of all the data.
Measurement bias: (1) Lysholm score: The subjectivity of assessment tools, such as the Lysholm score, can lead to measurement bias. Here, to reduce this bias, experienced physicians independently conducted all the ratings, which underwent a secondary review if necessary to ensure consistency. (2) VAS score: The VAS score has a certain degree of subjectivity and can be influenced by a patient’s feelings and expectations. To reduce this bias, VAS scores were recorded multiple times at different time points and they were then evaluated by the same doctor to improve the consistency and reliability of the scores.
Confounding factors: (1) Experience and technical level of the surgeon: Although all the surgeries were performed by experienced surgeons, the operational skills and experience of different doctors can affect the surgical results. To this end, we ensured that all the surgeries were performed by experienced surgeons in the same team to minimize technical differences between cases. (2) Consistency and compliance of postoperative rehabilitation plan: Although we strove to ensure that all the patients followed the same rehabilitation plan, individual differences and differences in compliance can have an impact on the final functional recovery. Therefore, in the data analysis, we considered the impact of these factors.
Statistical analysis
Data analysis was performed using SPSS 26.0 statistical software. Quantitative data were presented as the mean ± standard deviation (Mean ± SD), while count data were depicted as percentages. The paired t-test was employed to compare the mean values between the two groups (for quantitative data that followed a normal distribution). To compare rates between the two groups, either the χ2 test or the exact probability method was utilized. The t-test was employed for evaluating variations in the scores of the diverse surgical treatment outcomes. The surgical time, postoperative fracture alignment, fracture-healing time, changes in the range of motion, as well as postoperative Lysholm and VAS scores, were recorded and compared between the two groups. Statistical analysis was performed by both the first author and the corresponding author. Both authors have expertise and experience in statistical analysis and their agreement validated the results and ensured accuracy during the data analysis. Statistical significance was established at a threshold of P < 0.05.
Results
General condition of the patients
In total, 46 patients were enrolled in the study, comprising 28 males and 18 females (Table 1). The median age was 29 years old (range: 15–69). The median interval between the initial assessment and surgery was 12.7 days (range: 2–20). All the patients exhibited favorable healing of their surgical incisions postoperatively, with no instances of nerve or vascular impairment, as well as no occurrences of deep vein thrombosis. Notably, there were no instances of complications, such as infection, internal fixation failure, or fracture nonunion. Upon the final follow-up, all patients displayed normal postoperative walking gaits without discernible abnormalities. Both groups demonstrated the absence of significant limitations in flexion or extension and achieved the resumption of their preoperative occupational and daily activities (Fig. 1). There existed no noteworthy disparity in general characteristics between the two groups when comparing the Lysholm knee scores. General information on the two groups of patients, also showing the advantages and shortcomings of ORIF and arthroscopic surgery, is provided in Table S1.
| Characteristics | Arthroscopy group (n = 33) | ORIF group (n = 13) | p-value |
|---|---|---|---|
| Gender | |||
| Male | 18 (54.55%) | 10 (76.92%) | 0.168636165 |
| Female | 15 (45.45%) | 3 (23.08%) | |
| Meyer–McKeever type | |||
| II | 14 (42.42%) | 7 (53.85%) | |
| III | 19 (57.58%) | 6 (46.15%) | |
| Age | 47.97 ± 14.77 | 43.62 ± 15.07 | 0.37544344 |
| Waiting time before surgery (days) | 7.42 ± 4.49 | 7.15 ± 5.37 | 0.862718085 |
| Limping (points) | 3.15 ± 0.87 | 3.46 ± 0.88 | 0.283620649 |
| Assistive device assistance (points) | 2.91 ± 1.4 | 2.31 ± 1.32 | 0.189319021 |
| Joint strangulation (points) | 10.27 ± 4.48 | 10.62 ± 3.82 | 0.809326923 |
| Joint instability (points) | 8.03 ± 3.52 | 7.69 ± 2.59 | 0.755570645 |
| Joint swelling (points) | 2.79 ± 2.18 | 1.85 ± 1.52 | 0.161205537 |
| Upstairs (points) | 3.58 ± 1.98 | 3.54 ± 2.03 | 0.954752959 |
| Squatting (points) | 2.30 ± 1.24 | 2.62 ± 0.96 | 0.418588458 |
| Joint pain (points) | 7.42 ± 3.56 | 6.15 ± 2.19 | 0.238484302 |
| Total score (points) | 40 ± 14.8 | 37.69 ± 9.38 | 0.605382895 |
| VAS (points) | 3 ± 1.06 | 3.62 ± 0.96 | 0.076055646 |
Note:
ORIF, open reduction and internal fixation; VAS, Visual analogue scale.
Figure 1: A 53-year-old female with a posterior cruciate ligament tibial avulsion fracture in the left knee.
(A and B) Preoperative anteroposterior and lateral X-rays; (C and D) preoperative MRI and CT scans with three-dimensional reconstruction; (E and F) immediate postoperative lateral X-rays showing good fracture reduction; (G–I) bone healing and knee stabilization 12 months after surgery.Pre- and postoperative indicators in the arthroscopic group
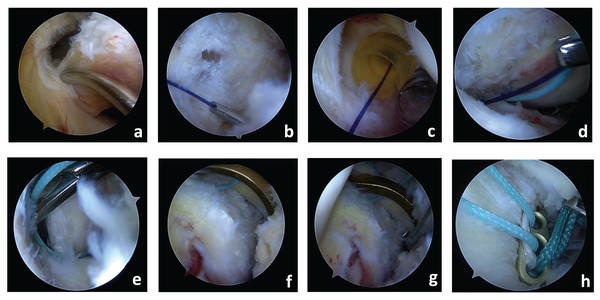
Figure 2 shows images of the arthroscopy surgery procedure. Following surgery, the patients in the arthroscopic group displayed satisfactory recovery outcomes (Table 2). Analysis of the Lysholm scores revealed a notable elevation in all eight indicators within the arthroscopic group (all P < 0.001). Additionally, the overall Lysholm score exhibited a significant enhancement from before to after surgery (P < 0.001). As for the VAS score, the patient average scores decreased from three points prior to surgery to 0.6 points following surgery (P < 0.001).
Figure 2: Images of the arthroscopy surgery procedure.
(A) The suture hook is passed through the posterior cruciate ligament at the base of the tibial insertion; (B) the suture hook is then passed through the base of the tibial insertion of the posterior cruciate ligament with stringing; (C) double posteromedial approach; (D) PDS-II stringing; (E) After suturing, the wire is wrapped around the root of the posterior fork ligament following insertion; (F) the tibial tunnel is located; (G) a hole is drilled in the bone marrow and the steel wire is threaded through it; (H) the loop steel plate is inserted and the high-strength wire is tightened for fixation.| Characteristics (points) | Pre-operative (n = 33) |
Post-operative (n = 33) |
p-value |
|---|---|---|---|
| Limping | 3.15 ± 0.87 | 4.76 ± 0.66 | 5.57E−12 |
| Assistive device assistance | 2.91 ± 1.4 | 4.91 ± 0.52 | 1.14E−10 |
| Joint strangulation | 10.27 ± 4.48 | 15 ± 0 | 7.99E−08 |
| Joint instability | 8.03 ± 3.52 | 21.52 ± 2.33 | 3.63E−27 |
| Joint swelling | 2.79 ± 2.18 | 7.82 ± 2.02 | 3.10E−14 |
| Stair climbing | 3.58 ± 1.98 | 9.88 ± 0.7 | 1.05E−25 |
| Squatting | 2.3 ± 1.24 | 4.58 ± 0.5 | 2.52E−14 |
| Joint pain | 7.42 ± 3.56 | 21.97 ± 2.48 | 2.59E−28 |
| Total score | 40 ± 14.8 | 90.88 ± 4.53 | 7.44E−28 |
| VAS | 3 ± 1.06 | 0.61 ± 0.5 | 1.28E−17 |
Note:
VAS, Visual analogue scale.
Pre- and postoperative indicators in the ORIF group
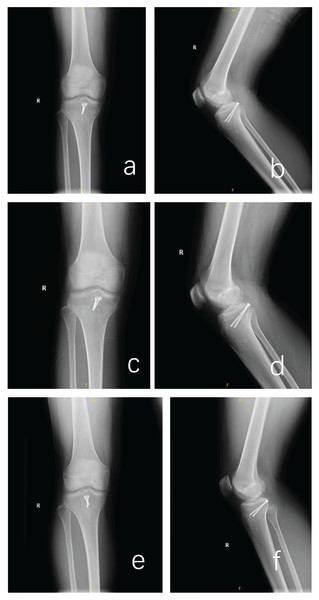
Figure 3 shows X-ray images taken after ORIF surgery. The patients in the ORIF group demonstrated marginally improved outcomes with respect to the preoperative limping and assistive device assistance indicators (P < 0.05, Table 3). Following surgery, the remaining six indicators exhibited substantial elevations (all P < 0.001). Furthermore, the total Lysholm score displayed a significant enhancement from before to after surgery (P < 0.001). In the context of the VAS score, the average patient score decreased from 3.6 points prior to surgery to 1.0 points post-surgery (P < 0.001).
Figure 3: Images of the control X-rays after ORIF surgery and images of the control X-rays at 1- and 3-months postoperative.
(A and B) X-ray images after ORIF surgery; (C and D) X-ray images 1 month after ORIF surgery; (E and F) X-ray images 3 months after ORIF surgery. Abbreviations: ORIF, open reduction and internal fixation.| Characteristics (points) | Pre-operative (n = 13) |
Post-operative (n = 13) |
p-value |
|---|---|---|---|
| Limping | 3.46 ± 0.88 | 4.54 ± 0.88 | 0.004542195 |
| Assistive device assistance | 2.31 ± 1.32 | 3.62 ± 1.56 | 0.029583248 |
| Joint strangulation | 10.62 ± 3.82 | 15 ± 0 | 0.000370775 |
| Joint instability | 7.69 ± 2.59 | 20.77 ± 1.88 | 1.63E−13 |
| Joint swelling | 1.85 ± 1.52 | 7.54 ± 2.03 | 2.50E−08 |
| Stair climbing | 3.54 ± 2.03 | 9.38 ± 1.5 | 1.44E−08 |
| Squatting | 2.62 ± 0.96 | 4.38 ± 0.51 | 4.65E−06 |
| Joint pain | 6.15 ± 2.19 | 20.38 ± 1.39 | 2.31E−16 |
| Total score | 37.69 ± 9.38 | 85.62 ± 4.39 | 1.05E−14 |
| VAS | 3.62 ± 0.96 | 1.08 ± 0.49 | 1.12E−08 |
Note:
ORIF, open reduction and internal fixation; VAS, Visual Analogue Scale.
Surgical outcomes in the two patient groups
Improvements across all indicators were observed in the patients in the arthroscopic group post-surgery (Table 4). Regarding the operating time, it was marginally longer in the arthroscopic group compared to the ORIF group. Notably, no substantial disparity in Lysholm scores of the knee joint existed between the two patient groups either prior to or following surgery (P > 0.05). This observation implies that both surgical approaches yielded noteworthy enhancements in knee function.
| Characteristics (Differences) | Arthroscopy group (n = 33) |
ORIF group (n = 13) |
p-value |
|---|---|---|---|
| Limping | 1.61 ± 1.06 | 1.08 ± 1.32 | 0.162016353 |
| Assistive device assistance | 2 ± 1.44 | 1.31 ± 2.18 | 0.212282001 |
| Joint strangulation | 4.73 ± 4.48 | 4.38 ± 3.82 | 0.809326923 |
| Joint instability | 13.48 ± 3.64 | 13.08 ± 3.25 | 0.726534815 |
| Joint swelling | 5.03 ± 3.21 | 5.69 ± 2.43 | 0.50589713 |
| Upstairs | 6.3 ± 2.01 | 5.85 ± 3.11 | 0.557088658 |
| Squatting | 2.27 ± 1.28 | 1.77 ± 1.01 | 0.211996078 |
| Joint pain | 14.55 ± 3.61 | 14.23 ± 2.77 | 0.779161793 |
| Total score | 50.88 ± 13.5 | 47.92 ± 9.13 | 0.472683377 |
| Limping | 2.39 ± 1.12 | 2.54 ± 1.20 | 0.7003 |
| Surgery time (minutes) | 68.21 ± 11.57 | 62.69 ± 17.39 | 0.215484641 |
Note:
ORIF, open reduction and internal fixation.
Discussion
Posterior cruciate ligament tibial avulsion fractures (PCLTAFs) are commonly managed according to the Meyers and McKeever classification (Meyers & McKeever, 1970). Within this classification, type I entails an avulsion fracture exhibiting minimal displacement, which is typically addressed through conservative strategies, like bracing or plaster fixation. Zhao (2015) proposed that a displacement of <5 mm could potentially be managed conservatively. In 2021, Yoon, Kim & Park (2021) reported 30 instances of PCLTAF and suggested that conservative management might be suitable for acute PCL avulsion fractures featuring a displacement of <6.7 mm. Type II in the Meyers and McKeever classification refers to a suspensory fracture wherein the avulsion fragment remains connected at one end while displaced at the other, while type III corresponds to a complete avulsion fracture with separation and displacement. Type IV involves complex fracture situations, including more extensive soft tissue injuries or damage to other associated structures. Types II, III, and IV fractures generally warrant surgical intervention. The surgical options encompass open reduction and internal fixation (ORIF) as well as arthroscopic reduction fixation, each offering distinct approaches and internal fixation choices (Li & Tian, 2015). In this investigation, both ORIF and arthroscopic reduction fixation yielded favorable clinical outcomes.
Open reduction and internal fixation (ORIF) encompasses a variety of techniques, including the modified posterior approach and medial approach. Within our surgical practice, the modified posterior approach is employed for ORIF procedures. This approach involves entry through the interval between the medial head of the gastrocnemius and the semitendinosus muscle, utilizing a smaller surgical incision. This approach not only facilitates superior visualization of the fracture site but also effectively avoids the posterior neural and vascular regions, thereby mitigating the risk of neural and vascular injuries. This approach is characterized by its simplicity, reduced tissue trauma, and consistent outcomes. However, our surgical team has observed that ORIF is more suitable for managing larger bone fragments than smaller or comminuted fractures. The excessive thickness of the cannulated screws can result in bone fragmentation during drilling and screw placement. In instances where the guiding needle’s positioning is suboptimal during nail fixation, repeated drilling can be necessary, extending the operation duration and potentially causing bone fragment crushing. Additionally, the bulky cannulated screws can lead to bone mass loss. Also, tension applied to the medial head of the gastrocnemius during surgery can result in postoperative gastrocnemius weakness, which could influence the range of motion of the knee joint. Moreover, the confined space behind the popliteal fossa can lead to postoperative scar tissue contracture, contributing to a reduced knee joint range of motion. Despite these limitations, based on the experience of our surgical team, ORIF can still provide consistent outcomes for suitable cases when the choice of internal fixation materials is appropriately made, also taking into account the size of the fracture fragments and the proficiency of the surgeon. However, prudent consideration should be given to the choice of internal fixation materials, accounting for the fracture fragment size and surgeon proficiency, to ensure selecting the most appropriate fixation material.
With advancements in arthroscopic techniques, the utilization of arthroscopic surgery for addressing PCLTAFs has surged, particularly for relatively minor avulsion fractures (Sundararajan et al., 2021a; Zhao et al., 2022). Our findings are consistent with those reported by Biz et al. (2019a), who found that arthroscopically assisted anterior cruciate ligament reconstruction showed good clinical and functional outcomes at interim follow-up. This further supports the use of arthroscopic techniques in knee surgery. In another study, Biz et al. (2019b) explored the long-term efficacy of tibial plateau fractures and found that early radiological features were predictive of the interim clinical functional outcomes. This suggests that future studies require longer follow-ups to assess the long-term efficacy and potential complications of arthroscopic techniques. Despite the present study’s findings that arthroscopy and open reduction yielded comparable clinical outcomes, our surgical team leans toward arthroscopic interventions for managing PCLTAFs in real-world clinical scenarios. Drawing from extensive clinical experience, we have indeed recognized several merits associated with the arthroscopic treatment of PCLTAFs: (1) It entails minimal trauma and requires only a small surgical incision, thereby effectively averting or mitigating potential neurovascular damage. Also, postoperative patients tend to exhibit rapid recovery and can commence early rehabilitation training; (2) the procedure is straightforward, offering a well-defined surgical field and precision in execution, thereby averting fracture fragmentation associated with cannulated screw usage and ensuring dependable fracture fixation. Comparable biomechanical strength is achieved compared to cannulated screw fixation, and the necessity for secondary surgery to extract the cannulated screws is eliminated; (3) it can facilitate the simultaneous detection and management of meniscal injury, cartilage injury, anterior cruciate ligament issues, and other intra-articular injuries; (4) the minimized exposure and thus risk of harm to the joint capsule, muscles, and fascial structures contribute to the reduction of postoperative soft tissue scarring; (5) suture fixation at the root of the tibial insertion point of the posterior cruciate ligament can enhance resistance against the loosening of the avulsed bone block, rendering it suitable for comminuted fractures and fractures featuring small bone pieces; (6) suture and loop plate fixation fall within the realm of elastic fixation, allowing micro-movement of the fractured segment after fixation, aligning with the principles of biological fracture fixation; (7) sole reliance on a solitary bone tunnel suture, spanning from the root of the posterior cruciate ligament tibial insertion to medial joint anchor screw fixation at the tibial tubercle, obviates the need for multiple tunnel threading and thus curtails bone damage, thereby streamlining the operation time; (8) the surgical procedure obviates the necessity for repetitive X-fluoroscopy, thereby mitigating radiation hazards.
The incidence of PCLTAF in adolescents is relatively low. Additionally, due to the presence of unclosed epiphyseal plates, controversies persist regarding treatment approaches and fixation materials (Guo et al., 2022). Posterior approach ORIF surgery is associated with trauma and is insufficient for managing concurrent comorbid injuries. In cases of severely crushed fractures, achieving robust fixation is challenging, and the early initiation of functional exercises is typically impeded, thereby influencing the recovery of the postoperative joint function. Arthroscopic treatment of PCLTAF in adult patients has demonstrated favorable outcomes (Ren et al., 2022). However, in adolescent patients, even with minimally invasive arthroscopic techniques, the risk of iatrogenic injury to the epiphyseal plate is elevated (Scarcella et al., 2021; Liu et al., 2023). Consequently, treatment in this population presents challenges. Literature reports exist regarding the utilization of cannulated screws and sutures passed through bone tunnels for addressing children’s PCLTAF without evident growth disorders during subsequent follow-up. The literature suggests that epiphyseal plate injuries below 5%, particularly those under 3%, are unlikely to arrest growth or induce limb deformities. However, when epiphyseal plate injuries escalate to 7%–9%, the likelihood of growth arrest or limb deformities becomes notably elevated (Brophy, Silverman & Lowry, 2023). Within the scope of this study, we employed a 3.5 mm cannulated screw for PCLTAF fixation. A solitary bone tunnel was created using a 4.5 mm hollow drill under arthroscopic guidance, which involved the removal of <1.6% of the epiphyseal plate, followed by fracture block fixation through the bone tunnel using a high-strength suture. Both surgical techniques yielded favorable outcomes, with epiphyseal injuries below 5%, thus fostering good patient recovery and facilitating robust bone healing. No occurrences of growth arrest or limb deformities were identified.
This study possesses certain limitations that merit consideration. First, the sample size of this study was relatively small, emphasizing the need to expand the sample size in subsequent investigations. Second, the follow-up time was relatively short, and additional observations are needed to determine long-term efficacy. Third, the inclusion of adolescent patients was limited, making it impossible to conduct stratified analysis of this subgroup. In addition, the patient cohort showed a wide age distribution (15 to 69 years old), and there is a risk that patients in different age groups may have different reactions to surgery and rehabilitation processes. Finally, there was a significant difference in sample size between the arthroscopic group (33 cases) and the ORIF group (13 cases), which may lead to bias in statistical analysis. Future studies will require larger samples and longer follow-ups to further validate these results, especially for ensuring the safety and long-term efficacy in adolescent patients.
Conclusion
In conclusion, arthroscopic suture fixation in conjunction with looped plate binding can significantly improve knee function and clinical effect for patients in the treatment of PCLTAF, helping improve postoperative functional recovery of patients. Future studies could further validate these results with larger samples and longer follow-ups, and explore their potential for application in different patient populations, providing patients with better treatment options and faster functional recovery.