Prognosis of hepatitis B virus reactivation in newly diagnosed multiple myeloma in modern era therapy: a retrospective study
- Published
- Accepted
- Received
- Academic Editor
- Priyanka Banerjee
- Subject Areas
- Virology, Gastroenterology and Hepatology, Hematology, Infectious Diseases, Oncology
- Keywords
- Hepatitis B virus, Reactivation, Multiple myeloma, Prognosis
- Copyright
- © 2024 Lv et al.
- Licence
- This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits using, remixing, and building upon the work non-commercially, as long as it is properly attributed. For attribution, the original author(s), title, publication source (PeerJ) and either DOI or URL of the article must be cited.
- Cite this article
- 2024. Prognosis of hepatitis B virus reactivation in newly diagnosed multiple myeloma in modern era therapy: a retrospective study. PeerJ 12:e18475 https://doi.org/10.7717/peerj.18475
Abstract
Studies on the prognosis of hepatitis B virus (HBV) reactivation following modern therapies for newly diagnosed MM (NDMM) are lacking. In this retrospective study, we aimed to assess the incidence, risk factors and prognosis of HBV reactivation in NDMM. A total of 33 of 355 patients with NDMM and HBV reactivation were included in this study. Multivariable analysis showed that hepatitis B surface antigen-positivity, hepatitis B core antibody-positivity, bortezomib-containing regimens, autologous stem cell transplantation, and gain of 1q21 were identified as independent risk factors of HBV reactivation in NDMM patients. The NDMM patients with HBV reactivation had poorer 3-year overall survival (OS) and progression-free survival (PFS) than did those without HBV reactivation, as confirmed by multivariate analysis. In conclusion, HBV reactivation in patients with NDMM constitutes a significant complication, correlating with reduced OS and PFS, and emerges as a potential adverse prognostic factor in the contemporary era of treatment.
Introduction
Infection caused by the hepatitis B virus (HBV), a virus that primarily affects the liver and lymphatic system, poses a significant global health challenge. China harbors a substantial population of individuals who exhibit chronic carriage of HBV, with numbers reaching into the millions (Guo et al., 2019). Several extrahepatic malignancies demonstrate associations with HBV infection (Kwok & Tran, 2016). Moreover, reactivation of the HBV is a well-documented adverse event commonly observed in individuals with hematologic malignancies undergoing or following cytotoxic drug-based chemotherapy. This reactivation, specifically, refers to an upregulation in the replication of HBV among individuals with latent HBV infection or those who have achieved successful remission from HBV infection (Wands, Chura & Roll, 1975). Furthermore, reactivation of the HBV can result in the onset of acute liver inflammation and impairment of hepatic functionality (Yeo et al., 2000; Hoofnagle, 2019) and significant complications of tumour chemotherapy and immunosuppressive therapy (Tsukune, Sasaki & Komatsu, 2019). In addition, growing evidence has demonstrated that HBV infection can influence the status of the host immune system and alter the response to tumour therapy (Lin, Chen & Huang, 2017; Sallberg & Pasetto, 2020; Wang, Zou & Liu, 2016; Carretero, Sektioglu & Garbi, 2015). Cytotoxic agent treatments, monoclonal antibody therapy, and bone marrow transplantation have been proven to be hazardous factors for HBV reactivation (Yeo et al., 2000; Yeo, Chan & Leung, 2009; Idilman & Arat, 2011).
Multiple myeloma (MM) is a malignant condition characterized by clonal proliferation of plasma cells, resulting in the presence of osteolytic lesions, decreased erythrocyte count, impaired renal function, and elevated levels of calcium in the blood (Tsukune, Sasaki & Komatsu, 2019). Notably, the occurrence of infection significantly contributes to the development of illness and mortality in patients with MM (Holmstrom, Gimsing & Abildgaard, 2015; Andersen, Klausen & Abildgaard, 2017), and HBV infection rates are higher in patients with MM than in those without. The increased predisposition to HBV infection in patients with MM is complex and related to multiple factors, such as congenital disease-related defects of the immune system or disease-associated adaptive immune system deficiency (Pratt, Goodyear & Moss, 2007; Brown, Pope & Murray, 2001). The application of novel treatments, including proteasome inhibitors, immunomodulation intervention, and monoclonal antibodies, has significantly prolonged the overall survival (OS) and progression-free survival (PFS) of patients with MM (Kumar, Rajkumar & Dispenzieri, 2008; Anderson, 2016). Meanwhile, the utilization of the aforementioned medications has been associated with an increasing prevalence of incidents related to HBV reactivation (Tsukune, Sasaki & Odajima, 2017; Atilla, Yalçıner & Atilla, 2019; International Myeloma Working Group, 2003; Huang, Li & Zhou, 2012; Stasi, Silvestri & Voller, 2017). Previous studies have shown that the prevalence of HBV reactivation ranging from 2% to 9% among individuals diagnosed with MM (Tsukune, Sasaki & Komatsu, 2019; Tsukune, Sasaki & Odajima, 2017; Atilla, Yalçıner & Atilla, 2019; Oketani, Ido & Uto, 2012; Lee, Lim & Lee, 2015; Tsukune, Sasaki & Odajima, 2016). However, the relationship between MM and HBV reactivation remains incompletely understood, with conflicting evidence regarding its impact on the prognosis of MM patients.
In this retrospective study, we sought to examine the occurrence of HBV reactivation and its related factors among individuals newly diagnosed with multiple myeloma (NDMM), while also evaluating the prognostic significance of HBV reactivation.
Methods
Patients
We retrospectively enrolled 412 Chinese patients with NDMM between 2015 and 2020 at the Sun Yat-sen University Cancer Center’s Department of Hematologic Oncology. None of the patients had received anti-tumor treatment previously. Among these 412 patients with NDMM, 57 cases were excluded due to lack of detection data of HBV. Finally, 355 patients were included in our analysis. The MM diagnosis relied on the criteria established by the International Myeloma Working Group (IMWG). The research has received approval from the Sun Yat-sen university cancer prevention and control center for ethics committee (ethical approval referenced number: B2023-471-01). The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation was not required from the participants or the participants’ legal guardians/next of kin in accordance with the national legislation and institutional requirements. The utilization of electronic health records was employed for the examination of patients’ information.
Patients’ characteristics and initial laboratory parameters were documented upon the commencement of chemotherapy (Table S1). The HBV infection-related data included hepatitis B surface antigen (HBsAg), hepatitis B core antibody (HBcAb), hepatitis B surface antibody (HBsAb), hepatitis B e-antigen (HBeAg), and hepatitis B e-antibody (HBeAb), and HBV DNA titers. Continuous monitoring of all patients was conducted throughout the study, with the exception of cases where patients could not be traced for follow-up until 31 December 2022 or they had passed away.
Measurements and definitions
HBsAg, HBcAb, HBsAb, HBeAg, and HBeAb were detected by chemiluminescence. Quantitative PCR was utilized to determine the titers of HBV DNA. HBV reactivation was defined as follows: (1) reappearance of HBsAg and loss of HBsAb in patients who were HBsAg-negative and/or HBsAb-positive; (2) increase of HBV DNA level by at least a factor of 10 in HBV DNA levels compared to the initial levels, or an absolute count of HBV DNA reaching 1 × 109 copies/mL In our study, we only analyzed HBV reactivation which occurred before the first progression of NDMM. Overall survival (OS) definition was that time from transplantation to death or date of last follow-up in alive patients. Progression-free survival (PFS) is defined as the time between the NDMM patients received initiation of treatment to disease progression or death from any cause.
Treatment
First-line regimens were as follows (Table 1): cyclophosphamide + thalidomide + dexamethasone (CTD, N = 19); bortezomib + adriamycin + dexamethasone (PAD, N = 140); ixazomib + lenalidomide + dexamethasone (IRD, N = 11); bortezomib + cyclophosphamide + dexamethasone (VCD, N = 16); liposomal doxorubicin + vincristine + dexamethasone (DVD, N = 53); bortezomib + dexamethasone (VD, N = 5); vincristine + doxorubicin + dexamethasone (VAD, N = 24); bortezomib + lenalidomide + dexamethasone (VRD, N = 78) and bortezomib + thalidomide + dexamethasone (VTD, N = 9). A total of 62 patients received autologous stem cell transplantation (ASCT) subsequent to undergoing high-dose chemotherapy. In patients with chronic HBV infection, treatment with entecavir (ETV), tenofovir disoproxil fumarate (TDF), tenofovir alafenamide fumarate (TAF), or tenofovir amibufenamide (TMF) for a duration of 48 weeks is recommended. If HBV DNA remains detectable after 48 weeks of therapy (HBV DNA > 20 IU/ml), adjustments can be made to the medication treatment plan, excluding errors related to compliance and detection. Patients currently prescribed ETV should consider transitioning to TDF or TAF, while those on TDF or TAF may consider switching to ETV; alternatively, a combination therapy involving both drugs can be considered. In patients with active HBV infection, treatment with ETV, TDF or TAF is recommended and the most appropriate antiviral regimen were selected according to the patient’s specific drug resistance.
| Characteristic | HBV reactivation status | P-value | ||
|---|---|---|---|---|
| Negative n (%) | Positive n (%) | |||
| A. Univariate analysis | ||||
| Number of patients | 322 | 33 | ||
| Age, n (%) | 0.356 | |||
| <65 years | 240 (75%) | 27 (82%) | ||
| ≥65 years | 82 (25%) | 6 (18%) | ||
| Sex, n (%) | 0.631 | |||
| Male | 201 (64%) | 22 (67%) | ||
| Female | 121 (36%) | 11 (33%) | ||
| MM subtype, | 0.145 | |||
| IgG | 198 (61%) | 14 (43%) | ||
| IgA | 77 (24%) | 10 (30%) | ||
| Light chain | 25 (8%) | 5 (15%) | ||
| aOthers | 22 (7%) | 4 (12%) | ||
| DS stage | 0.969 | |||
| I | 72 (22%) | 8 (24%) | ||
| II | 79 (25%) | 8 (24%) | ||
| III | 171 (53%) | 17 (52%) | ||
| ISS | 0.439 | |||
| 1 | 89 (28%) | 12 (36%) | ||
| 2 | 70 (22%) | 8 (24%) | ||
| 3 | 163 (50%) | 13 (40%) | ||
| R-ISS | 0.185 | |||
| 1 | 84 (26%) | 13 (39%) | ||
| 2 | 195 (61%) | 18 (55%) | ||
| 3 | 43 (13%) | 2 (6%) | ||
| IMWG risk stratification | 0.227 | |||
| Low risk | 77 (24%) | 12 (36%) | ||
| Moderate risk | 221 (69%) | 20 (61%) | ||
| High risk | 24 (7%) | 1 (3%) | ||
| Number of bone lesions | 0.108 | |||
| None | 80 (25%) | 3 (9%) | ||
| 1 | 23 (7%) | 2 (6%) | ||
| ≥2 | 219 (68%) | 28 (85%) | ||
| Plasma cells in bone marrow ≥10% | 0.251 | |||
| <10% | 180 (56%) | 15 (45%) | ||
| ≥10% | 142 (44%) | 18 (55%) | ||
| EMD | 0.240 | |||
| Yes | 29 (9%) | 1 (3%) | ||
| No | 293 (91%) | 32 (97%) | ||
| First-line regimens | 0.888 | |||
| VRD | 67 (21%) | 11 (33%) | ||
| VTD | 7 (2%) | 2 (6%) | ||
| VD | 5 (1%) | 0 (0%) | ||
| VCD | 14 (4%) | 2 (6%) | ||
| VAD | 22 (7%) | 2 (6%) | ||
| PAD | 125 (39%) | 15 (46%) | ||
| IRD | 11 (3%) | 0 (0%) | ||
| DVD | 53 (17%) | 0 (0%) | ||
| CTD | 18 (6%) | 1 (3%) | ||
| bUse of bortezomib | 0.006 | |||
| Yes | 218 (68%) | 30 (91%) | ||
| No | 104 (32%) | 3 (9%) | ||
| bUse of thalidomide | 0.369 | |||
| Yes | 92 (29%) | 7 (21%) | ||
| No | 230 (71%) | 26 (79%) | ||
| bUse of lenalidomide | 0.036 | |||
| Yes | 153 (48%) | 22 (67%) | ||
| No | 169 (52%) | 11 (33%) | ||
| bASCT | 0.003 | |||
| Yes | 50 (16%) | c12 (36%) | ||
| No | 272 (84%) | 21 (64%) | ||
| Chromosomal aberrations | ||||
| 1q21+ | 48 (15%) | 10 (30%) | 0.023 | |
| 13q14− | 34 (11%) | 1 (3%) | 0.167 | |
| IGH rearrangements | 15 (5%) | 1 (3%) | 0.668 | |
| P53− | 19 (6%) | 1 (3%) | 0.496 | |
| dHBsAg | <0.0001 | |||
| Positive | 21 (7%) | 14 (42%) | ||
| Negative | 301 (93%) | 19 (58%) | ||
| dHBsAb | 0.014 | |||
| Positive | 202 (63%) | 13 (39%) | ||
| Negative | 120 (37%) | 20 (61%) | ||
| dHBcAb | <0.0001 | |||
| Positive | 157 (49%) | 29 (88%) | ||
| Negative | 165 (51%) | 4 (12%) | ||
| dHBeAg | 0.012 | |||
| Positive | 3 (1%) | 3 (9%) | ||
| Negative | 319 (99%) | 30 (91%) | ||
| dHBeAb | 0.224 | |||
| Positive | 85 (26%) | 12 (36%) | ||
| Negative | 237 (74%) | 21 (64%) | ||
| Died | 0.016 | |||
| Yes | 75 (23%) | 14 (42%) | ||
| No | 247 (77%) | 19 (58%) | ||
| Progression of MM | 0.001 | |||
| Yes | 111 (34%) | 21 (64%) | ||
| No | 211 (66%) | 12 (36%) | ||
| Parameter | Multivariate analysise | ||
|---|---|---|---|
| HR | 95% confidence interval | P-value | |
| B. Multivariate analysis | |||
| fHBsAg | 5.584 | [2.686–11.606] | <0.0001 |
| fHBcAb | 4.899 | [1.646–14.584] | 0.004 |
| gUse of bortezomib | 4.222 | [1.278–13.945] | 0.018 |
| gASCT | 2.751 | [1.330–5.687] | 0.006 |
| 1q21+ | 2.752 | [1.250–6.055] | 0.012 |
Notes:
MM, multiple myeloma; Ig, immunoglobulin; DS, Durie-Salmon; ISS, International Staging System; R-ISS, Revised-International Staging System; IMWG, International Myeloma Working Group; EMD, extramedullary disease; HBV, hepatitis B virus; ASCT, autologous stem cell transplantation; IGH, human immunoglobulin heavy chains; VRD, bortezomib + lenalidomide + dexamethasone; VTD, bortezomib + thalidomide + dexamethasone; VD, bortezomib + dexamethasone; VCD, bortezomib + cyclophosphamide + dexamethasone; VAD, vincristine + doxorubicin + dexamethasone; PAD, bortezomib + adriamycin + dexamethasone; IRD, ixazomib + lenalidomide + dexamethasone; DVD, liposomal doxorubicin + vincristine + dexamethasone; cyclophosphamide + thalidomide + dexamethasone, CTD; ASCT, autologous stem cell transplantation.
Statistical analyses
The results were performed by IBM SPSS Statistics 25.0. The median values, accompanied by their corresponding ranges, were presented to depict the numerical data. The comparison of categorical variables involved the utilization of either Pearson chi-square test or Fisher exact test. The factors influencing HBV reactivation rates were analyzed using a chi-square test in a univariate analysis. Multivariate analysis used Cox regression to further evaluate the hazard elements. The Kaplan-Meier method was performed to analyze OS. Cumulative incidence was applied to calculate the incidence of HBV reactivation and progression of NDMM using competing risk model, and the death was seen as a risk of competition. The utilization of two-sided P-values was employed. The statistical significance was determined when the P-value was less than 0.05. Competitive risk model in R method (R version 4.2.1; R Core Team, 2022) was used to analyze the cumulative incidence.
Results
Patients’ characteristics
In our study, 355 patients (223 males and 132 females) were enrolled. The age distribution of the confirmed cases ranged from 24 to 85 years, with a median age of 58 years. The duration of follow-up ranged from 0 to 104 months, with a median of 44.0 months. The fundamental attributes of the enrolled patients are summarized in Table S1. Among the patients, 152 showed HbsAg-negativity combined with HBcAb-positivity and all of these individuals were administered entecavir (0.5 mg qd) as a prophylactic measure against HBV reactivation. In addition, 35 patients had confirmed HBV infection at diagnosis of MM characterized by HBsAg-positivity, as indicated by the presence of HBsAg, and all these patients received entecavir (0.5 mg qd) for anti-HBV therapy.
Morbidity and hazard elements of HBV reactivation before the first progression of NDMM
Among the 355 patients enrolled in our analysis, 33 (9.3%) developed HBV reactivation before the first progression of NDMM, with a median HBV reactivation time of 3 months (range, 0–31 months). The characteristics of the 33 patients with HBV reactivation including transaminases and HBV DNA copies were shown in Table S2. The 2- and 5-year overall cumulative incidences of HBV reactivation before the first progression of NDMM were 9.1% (95% confidence interval (CI) [5.96–12.24%]) and 9.9% (95% CI [6.76–13.04%]), respectively. Univariable analysis showed that bortezomib-containing regimens (P = 0.006), lenalidomide treatment (P = 0.036), ASCT (P = 0.003), 1q21+ (P = 0.023), HBsAg-positivity (P < 0.0001), HBsAb-positivity (P = 0.014), HBcAb-positivity (P < 0.0001), and HBeAg-positivity (P = 0.012) were hazard elements of HBV reactivation before the first progression of NDMM (Table 1A). Multivariable analysis showed that HBsAg-positivity (P < 0.0001, hazard ratio [HR] 5.584, 95% CI [2.686–11.606]), HBcAb-positivity (P = 0.004, [HR] 4.899, 95% CI [1.646–14.584]), bortezomib-containing regimens (P = 0.018, [HR] 4.222, 95% CI [1.278–13.945]), ASCT (P = 0.006, [HR] 2.751, 95% CI [1.330–5.687]), and 1q21+ (P = 0.012, [HR] 2.572, 95% CI [1.250–6.055]) were identified as independent hazard elements of HBV reactivation (Table 1B).
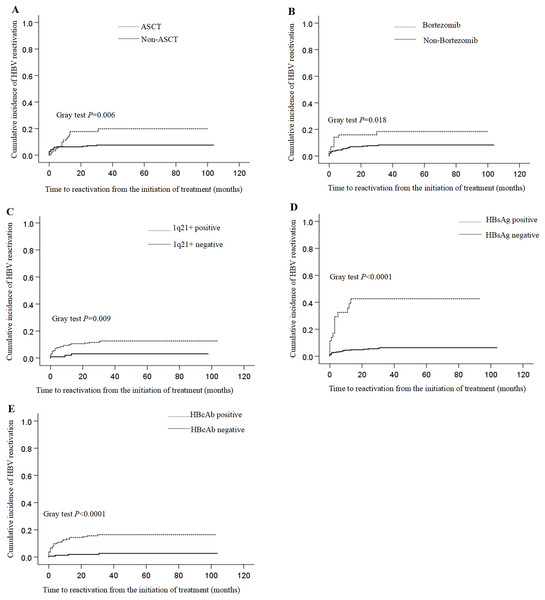
The occurrence of HBV reactivation during a 2-year period in patients who underwent ASCT (17.7%, 95% CI [8.10–27.30%]) was higher than that in patients who did not undergo ASCT (4.5%, 95% CI [0.21–6.85%]; P = 0.006) (Fig. 1A). The 2-year cumulative incidence of HBV reactivation in patients receiving bortezomib-containing regimens (11.8%, 95% CI [7.88–15.72%]) was higher than that in patients not receiving bortezomib-containing regimens (3.1%, 95% CI [0.43–6.63%]; P = 0.018) (Fig. 1B). Furthermore, the cumulative incidence of HBV reactivation during a 2-year period in patients with 1q21+ (15.9%, 95% CI: 6.30–25.50%) was higher than that of those without 1q21+ (7.7%, 95% CI [4.56–10.84%]; P = 0.009) (Fig. 1C). The 2-year cumulative incidence of HBV reactivation in patients with HBsAg-positivity (42.6%, 95% CI [25.55–59.65%]) was higher than that of those with HBsAg negative (5.5%, 95% CI [2.95–8.05%]; P < 0.0001) (Fig. 1D). Finally, the 2-year cumulative incidence of HBV reactivation in patients with HBcAb-positivity (15.6%, 95% CI [10.31%–20.89%]) was higher than that of those with HBcAb-negativity (1.9%, 95% CI [0.26–4.06%]; P < 0.0001) (Fig. 1E).
Figure 1: Cumulative incidences of HBV reactivation.
(A) Asessment of cumulative incidence of HBV reactivation in NDMM patients according to whether they received ASCT or not; (B) asessment of cumulative incidence of HBV reactivation in NDMM patients according to whether they received bortezomib-containing regimens or not; (C) asessment of cumulative incidence of HBV reactivation in NDMM patients according to whether they had gain of 1q21 or not; (D) asessment of cumulative incidence of HBV reactivation in NDMM patients according to whether they had HBsAg positive or not at initiation of treatment; (E) asessment of cumulative incidence of HBV reactivation in NDMM patients according to whether they had HBcAb positive or not at initiation of treatment.Survival analysis
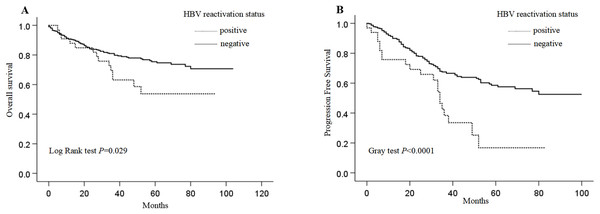
To analyse the relevance of the clinical parameters of patients with NDMM to their OS and PFS, we assessed multiple clinical data of patients with NDMM in Table 2. Of the 33 patients with HBV reactivation before the first progression of NDMM, 19 (58%) survived, and 14 (42%) died at a median follow-up of 40.0 months (range, 5–94 months) after HBV reactivation. Among these 14 patients, five (36%) died of treatment-related complications, including myocardial infarction (one case), septicaemia (two cases), and severe pneumonia (two cases), while nine (64%) died of complications of MM progression. None of the 33 patients with HBV reactivation developed fulminant hepatitis, and none of them experience MM-related treatment withdrawn. The patients with HBV reactivation had poorer 3-year survival than did those without HBV reactivation (63.1 ± 8.5% vs 81.0 ± 2.2%, P = 0.029) (Fig. 2A). Furthermore, univariate analysis revealed that International Staging System (ISS), Revised-International Staging System (RISS), IMWG, ASCT, deletion of P53, progression, and HBV reactivation were significant hazard elements for OS (Table 2; P < 0.05). Multivariable analysis showed that R-ISS stage, IMWG risk stratification, progression of NDMM, and HBV reactivation were identified as independent hazard elements of OS (Table 3A).
| Characteristic | Median OS, months | P-value | Median PFS, months | P-value | |
|---|---|---|---|---|---|
| Age | 0.288 | 0.893 | |||
| <65 years | 46.0 | 33.0 | |||
| ≥65 years | 39.5 | 30.0 | |||
| Sex, n (%) | 0.545 | 0.803 | |||
| Male | 41.0 | 32.0 | |||
| Female | 48.5 | 35.0 | |||
| MM subtype, | 0.205 | 0.598 | |||
| IgG | 44.5 | 35.5 | |||
| IgA | 44.0 | 28.0 | |||
| Light chain | 45.5 | 32.5 | |||
| aOthers | 44.5 | 31.5 | |||
| DS stage | 0.308 | 0.036 | |||
| I | 41.0 | 33.5 | |||
| II | 39.0 | 33.0 | |||
| III | 46.0 | 33.0 | |||
| ISS | 0.001 | 0.360 | |||
| 1 | 48.0 | 33.0 | |||
| 2 | 46.5 | 32.5 | |||
| 3 | 43.0 | 34.0 | |||
| R-ISS | <0.0001 | 0.046 | |||
| 1 | 48.0 | 38.0 | |||
| 2 | 44.0 | 33.0 | |||
| 3 | 34.0 | 28.0 | |||
| IMWG risk stratification | <0.0001 | 0.014 | |||
| Low risk | 47.0 | 36.0 | |||
| Moderate risk | 44.0 | 33.0 | |||
| High risk | 22.0 | 21.0 | |||
| Number of Bone lesions | 0.778 | 0.149 | |||
| None | 49.0 | 39.0 | |||
| 1 | 71.0 | 35.0 | |||
| ≥2 | 41.0 | 30.0 | |||
| Plasma cells in BM ≥ 10% | 0.773 | 0.129 | |||
| <10% | 43.5 | 34.0 | |||
| ≥10% | 45.0 | 31.0 | |||
| EMD | 0.776 | 0.376 | |||
| Yes | 43.0 | 30.0 | |||
| No | 68.0 | 33.0 | |||
| bUse of bortezomib | 0.130 | 0.702 | |||
| Yes | 42.0 | 33.0 | |||
| No | 61.0 | 32.0 | |||
| bUse of thalidomide | 0.692 | 0.006 | |||
| Yes | 67.0 | 32.0 | |||
| No | 40.0 | 33.0 | |||
| bUse of lenalidomide | 0.321 | 0.019 | |||
| Yes | 39.0 | 33.0 | |||
| No | 58.5 | 32.5 | |||
| bASCT | 0.028 | 0.103 | |||
| Yes | 40.0 | 34.0 | |||
| No | 45.0 | 32.0 | |||
| Chromosomal aberrations | |||||
| 1q21+ | 0.070 | 0.003 | |||
| Yes | 39.0 | 21.0 | |||
| No | 45.0 | 33.0 | |||
| 13q14− | 0.061 | 0.015 | |||
| Yes | 45.0 | 26.0 | |||
| No | 44.0 | 33.0 | |||
| IGH rearrangements | 0.178 | 0.007 | |||
| Yes | 45.0 | 29.0 | |||
| No | 44.0 | 33.0 | |||
| P53- | <0.0001 | 0.004 | |||
| Yes | 21.5 | 19.5 | |||
| No | 45.0 | 33.0 | |||
| HBV reactivation | 0.029 | <0.0001 | |||
| Yes | 40.0 | 31.0 | |||
| No | 45.0 | 33.0 | |||
| Progression of MM | 0.001 | — | |||
| Yes | 41.0 | — | |||
| No | 48.5 | — | |||
Notes:
MM, multiple myeloma; Ig, immunoglobulin; DS, Durie-Salmon; ISS, International Staging System; R-ISS, Revised-International Staging System; IMWG, International Myeloma Working Group; BM, bone marrow; EMD, extramedullary disease; HBV, hepatitis B virus; ASCT, autologous stem cell transplantation.
Figure 2: Overall survival (OS) and progression free survival (PFS) of patients with and without HBV reactivation.
(A) OS of HBV reactivation or not in patients with NDMM; (B) OS of HBV reactivation or not in patients with NDMM.| A. Overall survival | ||||
|---|---|---|---|---|
| Parameter | Multivariate analysisa | |||
| HR | 95% confidence interval | P-value | ||
| IMWG risk stratification | 0.008 | |||
| Low risk | — | — | — | |
| Moderate risk | 1.781 | [0.781–4.061] | 0.170 | |
| High risk | 4.356 | [1.550–12.236] | 0.005 | |
| HBV reactivation | 2.127 | [1.174–3.851] | 0.013 | |
| Progression of MM | 1.622 | [1.056–2.490] | 0.027 | |
| R-ISS | 0.041 | |||
| 2 | — | — | — | |
| 1 | 1.02 | [0.477–2.183] | 0.959 | |
| 3 | 2.049 | [1.171–3.586] | 0.012 | |
| B. Progression-free survival | |||
|---|---|---|---|
| Parameter | Multivariate analysisa | ||
| HR | 95% confidence interval | P-value | |
| HBV reactivation | 2.936 | [1.812–4.759] | <0.001 |
| bUse of lenalidomide | 0.542 | [0.375–0.783] | 0.001 |
| 1q21+ | 2.427 | [1.189–4.956] | 0.015 |
| P53- | 2.256 | [1.138–4.472] | 0.020 |
Notes:
IMWG, International Myeloma Working Group; HBV, hepatitis B virus; MM, multiple myeloma; R-ISS, Revised-International Staging System; IGH, Human immunoglobulin heavy chains.
Of the 33 patients with HBV reactivation before the first progression of NDMM, 21 (64%) developed NDMM progression at a median follow-up of 31.0 months (range, 0–83 months). The other 12 (36%) patients were free from disease progression, including two patients who died before primary disease progression. Moreover, the patients with HBV reactivation had poorer 3-year PFS than did those without HBV reactivation (38.4 ± 9.4% vs. 67.5 ± 2.8%, P < 0.0001) (Fig. 2B). Univariate analysis showed that DS, R-ISS, IMWG, use of thalidomide or lenalidomide, 1q21+, Immunoglobulin Heavy Chain (IGH) rearrangements, deletion of 13q14, deletion of P53, and HBV reactivation were significant hazard elements for PFS (Table 3; P < 0.05). Multivariable analysis showed that HBV reactivation, use of lenalidomide, deletion of P53 and 1q21+ were identified as independent hazard elements of PFS (Table 3B).
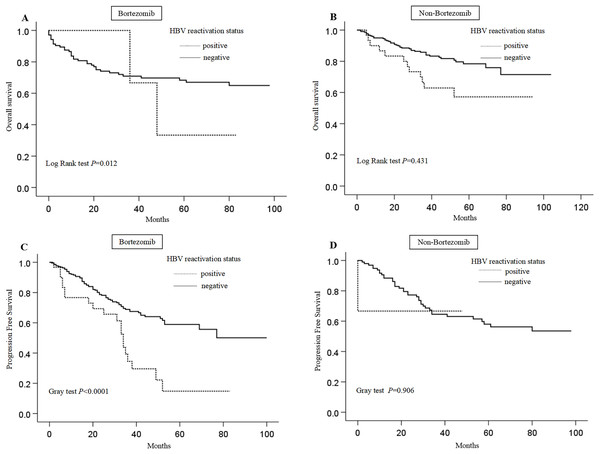
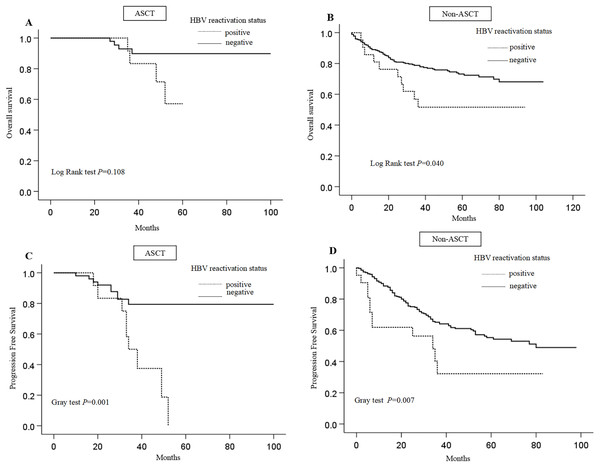
Considering the therapeutic regimen’s impact on survival, patients were categorised into four cohorts: those receiving ASCT, those not receiving ASCT, and those treated with bortezomib-containing regimens, and those without such treatment. Subsequently, we examined the effect of HBV reactivation on OS and PFS. HBV-reactivated patients had a significantly shorter OS (P = 0.012) and PFS (P < 0.0001) than non-HBV-reactivated patients, in the group receiving bortezomib-containing regimens (Figs. 3A, 3C). In contrast, there was no significant difference in either OS or PFS between HBV-reactivated and non-HBV-reactivated patients in the group without bortezomib-containing regimens (Figs. 3B, 3D). HBV-reactivated patients had a significantly shorter OS than did non-HBV-reactivated patients in the group without ASCT (P = 0.040). In comparison, there was no statistical significance in the Kaplan–Meier curves between HBV-reactivated patients and non-HBV-reactivated patients in the group with ASCT despite a trend of shorter OS, which might be because of the insufficient sample size (Figs. 4A, 4C). Finally, HBV-reactivated patients had significantly shorter PFS than non-HBV-reactivated patients in both groups with (P = 0.001) and without ASCT (P = 0.007) (Figs. 4B, 4D).
Figure 3: Impact of HBV reactivation on survival of patients with NDMM receiving bortezomib-containing regimens or not.
(A) OS of HBV reactivation or not in patients receiving bortezomib-containing regimens; (B) OS of HBV reactivation or not in patients not receiving bortezomib-containing regimens; (C) PSF of HBV reactivation or not in patients receiving bortezomib-containing regimens; (D) PFS of HBV reactivation or not in patients not receiving bortezomib-containing regimens.Figure 4: Impact of HBV reactivation on survival of patients with NDMM receiving ASCT or not.
(A) OS of HBV reactivation or not in patients receiving ASCT; (B) OS of HBV reactivation or not in patients not receiving ASCT; (C) PSF of HBV reactivation or not in patients receiving ASCT; (D) PFS of HBV reactivation or not in patients not receiving ASCT.Discussion
In this study, we assess the incidence and risk factors for HBV reactivation in NDMM and to further explore the prognosis of patients with HBV reactivation. Our result showed that HBV reactivation in patients with NDMM constitutes a significant complication, correlating with poor OS and PFS.
Our current research showed that the incidence of HBV reactivation was 9.3%, which was consistent with previous studies. The identification of hazard elements associated with HBV reactivation in patients diagnosed with NDMM remains elusive. Our results showed that HBsAg/HBcAb positivity at the initial stage of chemotherapy, ASCT, bortezomib-containing regimens, and 1q21+ were independent hazard elements for HBV reactivation in patients with NDMM before the first progression. Notably, high-dose chemotherapy with ASCT is widely used to treat MM. However, ASCT is associated with profound deficiencies in the immune system function, and patients undergoing ASCT are susceptible to various infections. Consistent with our results, the potential risk of HBV reactivation associated with ASCT has been demonstrated by multiple studies (Tsukune, Sasaki & Odajima, 2017; Lee, Lim & Lee, 2015). Bortezomib is a proteasome inhibitor that suppresses T lymphocyte proliferation and decreases the function of natural killer cells as well as that of CD8-positive T cells (Nucci & Anaissie, 2009). Previous studies have suggested that the patients who received bortezomib-containing therapy had a higher incidence rate of HBV reactivation than did those who received conventional chemotherapy (Li et al., 2015), which is consistent with our results. Potential risk factors have been reported previously, including HBsAg positivity (Yeo et al., 2004) and HBcAb positivity (Papamichalis, Alexiou & Boulbou, 2012), which are concordant with our results.
Notably, our study demonstrated that 1q21+ were independent hazard elements for HBV reactivation in patients with NDMM which has not been previously reported. Previous data reported by Guo et al. (2019) showed that higher prevalence of 1q21+ in patients with MM who experienced HBV infection, suggesting a potential contribution of HBV infection to the amplification of 1q21, thereby contributing to the progression of MM. Diverging from the aforementioned study, the multivariate analysis in our study proved that 1q21+ was a contributor to HBV reactivation. However, the mechanism underlying the interaction between 1q21 and HBV reactivation requires further investigation.
The effects of HBV infection on the survival of patients with MM are controversial. Guo et al. (2019) and Li et al. (2015) showed that both the OS and PFS rates of patients with positive HBsAg who received ASCT were significantly lower than those of patients with negative HBsAg. Conversely, Atilla, Yalçıner & Atilla (2019) did not detect any advantages in OS or PFS in HBsAg-negative patients. Unlike the above studies, our present data were based on HBV reactivation before the first progression of NDMM rather than on the simple positive status of HBV. Surprisingly, HBV reactivation was shown to be an independent prognostic factor for both OS and PFS in patients with NDMM via multivariate prognostic analysis, which has not been reported previously. Considering the therapeutic regimen’s impact on outcomes, we conducted an analysis to assess the impact of HBV reactivation on OS and PFS in patients who underwent either bortezomib-containing regimens or ASCT. Notably, among patients receiving either bortezomib-containing regimens or ASCT, the OS and PFS of HBV-reactivated patients were shorter than those of non-HBV-reactivated patients. These results provide further evidence for poor outcomes in patients with HBV reactivation. Patients with HBV infection in an active state, HBV infection in an chronic state, or HBV reactivation received regular administration of antiviral therapy in the current investigation. None of the patients with HBV reactivation developed fulminant hepatitis, and the main cause of death was MM progression. Our multiparameter analysis showed that MM progression was an independent hazard element for OS, while HBV reactivation was an independent hazard element for PFS. Because lymphocytes are the most important target cells of HBV, we speculated that the host immune system might display a set of changes following long-term infection of lymphocytes by HBV, causing refractoriness to pharmacotherapy or evasion of immune response by MM cells and leading to MM progression and shorter OS. However, this hypothesis warrants further investigation. It is crucial to acknowledge that reactivation of HBV can occur at any phase of treatment and requires regular, long-term monitoring of HBV DNA levels. Additionally, a novel approach needs to be established in order to prevent HBV reactivation in MM patients.
There were some limitations in our study. First, this was a retrospective single-centre analysis, wherein the systematic search for HBV reactivation during follow-up was inadequate. Second, 13.8% (57/412) of patients were excluded from the analysis because of a lack of HBV detection data. Therefore, our study might not have accurately determined the incidence of HBV reactivation. Further retrospective multicentre studies are required to validate our results.
In conclusion, our study demonstrated that HBV reactivation in patients with NDMM is not an infrequent complication and is associated with reduced OS and PFS. Bortezomib-containing regimens, ASCT, and 1q21+ were independent hazard elements for HBV reactivation in patients with NDMM. Additional cohort studies are required to confirm these findings.
Clinical practice points
The application of novel treatments of MM, including proteasome inhibitors, immunomodulation intervention, and monoclonal antibodies, has significantly improved the prognosis of MM, but the utilization of the aforementioned medications has been associated with an increasing prevalence of incidents related to HBV reactivation.
Our study provides updated insights into the impact of HBV reactivation on the unfavorable prognosis of NDMM, particularly by significantly diminishing survival rates through its facilitation of disease progression rather than fatal hepatitis, thereby potentially influencing future clinical management and patient care strategies.
Supplemental Information
Study population characteristics.
aOthers include IgM, IgD, IgE and non-secretory myeloma. b Before the first progression. MM, multiple myeloma; Ig, immunoglobulin; DS, Durie-Salmon; ISS, International Staging System; R-ISS, Revised-International Staging System; IMWG, International Myeloma Working Group; EMD, extramedullary disease; HBV, hepatitis B virus; ASCT, autologous stem cell transplantation.
Summary of the 33 patients with HBV reactivation.
ALT, glutamic-pyruvic transaminase; AST, glutamic oxalacetic transaminase; TBIL, serum total bilirubin; ETV, entecavir, TDF, tenofovir disoproxil fumarate, TAF, tenofovir alafenamide fumarate.