Quality of care and prescription patterns among patients with diabetic kidney disease—a large-scale cohort study from Taiwanese clinics
- Published
- Accepted
- Received
- Academic Editor
- Gwyn Gould
- Subject Areas
- Diabetes and Endocrinology, Internal Medicine, Nephrology, Public Health
- Keywords
- Diabetic kidney disease, Sodium glucose cotransporter 2 inhibitor, Glucagon-like peptide-1 receptor agonist, ABC goal, Primary care, Diabetes mellitus
- Copyright
- © 2022 Tsai et al.
- Licence
- This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits using, remixing, and building upon the work non-commercially, as long as it is properly attributed. For attribution, the original author(s), title, publication source (PeerJ) and either DOI or URL of the article must be cited.
- Cite this article
- 2022. Quality of care and prescription patterns among patients with diabetic kidney disease—a large-scale cohort study from Taiwanese clinics. PeerJ 10:e13636 https://doi.org/10.7717/peerj.13636
Abstract
Aims
To investigate the quality of care and prescription patterns of patients with diabetic kidney disease (DKD) receiving primary care at local clinics in Taiwan.
Methods
A retrospective chart review was conducted in 43 primary care clinics in Taiwan. The patients’ baseline characteristics, laboratory tests, presence of complications and antidiabetic agents prescribed were analyzed.
Results
7,200 patients with type 2 diabetes mellitus were enrolled. Percentage of HbA1c, blood pressure (BP), and low density lipoprotein cholesterol (LDL-C) goals reached were 52.5% in HbA1c < 7%, 40.9% in BP < 130/80 mmHg and 79.7% in LDL-C < 2.59 mmol/L. 18.3% achieved all three ABC goals. However, patients with DKD had a lower rate of ABC goal attainment and higher rate of complications. Among DKD patients with eGFR ≥ 30 ml/min/1.73 m2 and on monotherapy, metformin was most frequently prescribed. As for dual therapy, the most common combinations were metformin with sulfonylurea and metformin with DPP-4 inhibitors.
Conclusions
Diabetes patients in Taiwan receiving primary diabetes care at local clinics had generally satisfactory management performance. However, more aggressive HbA1c, BP, and LDL-C management among DKD patients should be emphasized. Contrary to current recommendations, SGLT-2 inhibitors and GLP-1 receptor agonists as frontline therapy were under-prescribed.
Introduction
Type 2 diabetes is a major challenge for the healthcare system globally and locally; the prevalence of diabetes mellitus (DM) has increased from 4.7% in the 1980s to 8.5% in 2014 and is still rising (World Health Organization, 2016). The age-adjusted comparative prevalence of diabetes in Taiwan has grown from 9.1% in 2000 to 9.7% in 2021, and is expected to be 11.5% in 2030 (International Diabetes Federation, 2021). Patients with diabetes are at higher risk for microvascular and macrovascular complications, which result in heavy economic burden for the society. It was estimated that diabetes-related health expenditure was 1,314.0 USD per person (International Diabetes Federation, 2021). The aggregated expenditure of diabetes patients accounted for 29.7% of NHI expenditure.
Diabetic kidney disease (DKD) is one of the most common complications among type 2 diabetes. In Taiwan, DKD is the most common cause for ESRD. From 2005 to 2014, the prevalence of DKD patients increased from 10.5% to 17.9%, and were expected to grow as the diabetic population increases (Lin et al., 2019). Statistically, Taiwan has the highest incidence and prevalence of dialysis in the world (Lin et al., 2014).
Target attainment and routine assessment for HbA1c, blood pressure (BP) and low density lipoprotein cholesterol (LDL-C) among diabetes has long been advocated by the International Diabetes Federation (IDF) and American Diabetes Association (ADA) Guidelines (American Diabetes Association, 2012; IDF Clinical Guidelines Task Force, 2006). Multifactorial controls has been widely recognized in reducing complications and improving outcomes of diabetes (Chan et al., 2009b; Gaede et al., 2008; Tu et al., 2010). However, past reports showed general low HbA1c, BP, and LDL-C (ABC) target attainment. The Joint Asia Diabetes Evaluation Program found that among seven Asian countries only 5.4% diabetes achieving the ABC goals (So et al., 2011). And The International Diabetes Management Practices Study (IDMPS) found only 3.6% diabetes from 17 countries in Europe, Asia, Latin America and Africa achieving all ABC targets (Chan et al., 2009a). In Taiwan, survey data from the National Diabetes Health Promotion Centers reported only 30–35% achieving individual goals and 4.5% achieving all ABC goals (Yu et al., 2009).
To date, most studies regarding diabetes care in Taiwan were conducted at either medical centers or regional hospitals. Yet, 40% of diabetes population received care at local clinics; the report of quality of care at the primary care has been limited. Hence, this report sought to conduct a retrospective, cross-sectional study investigating the characteristics, goal attainment, complications, and prescription patterns among DKD patients at the primary medical care level in Taiwan.
Materials & Methods
Study design and study population
This study aimed to investigate the quality of care and prescription patterns of patients with DKD receiving primary care at local clinics in Taiwan.
A retrospective chart review was conducted among 43 primary care clinics located in northern, middle, and southern Taiwan. These primary care clinics were all registered members of the Diabetes Share Care Network, a government plan featuring a team-oriented and pay-for-performance (P4P) model operated by the Health Promotional Administration of Taiwan. To be registered as a member, the clinic is required to (1) provide multidisciplinary professional care consisting of doctors, nurses, and dietitians, and (2) follow-up on DM patients’ routine checkups. In its service patient pool of the P4P program, each clinic selected and enrolled 50–350 patients according to their service capacity with following methods.
In the study period (July to October 2019), each DM patient who visited one of the network’s clinics for diabetes management and fulfilled the inclusion criteria was enrolled in this study until each clinic achieved its maximum enrollment capacity. The inclusion criteria included: 1. Diagnosis of type 2 diabetes at least one year prior to the index day (index day: first DM clinic visit within the study period). 2. Age of 20 years and older. 3. Has made at least one DM visit within 3–6 months prior to the index day. Pregnant patients were excluded.
This study complied with the ethical principles of the Declaration of Helsinki and was reviewed and approved by the Institutional Review Board of Antai Medical Care Cooperation Antai Tian-Sheng Memorial Hospital. (TSMH IRB No. 19-106-B)
Data collection
At each DM checkup (including index day), the patient’s baseline characteristics, physical examination, laboratory examinations, presence of complications and antidiabetic agents prescribed were recorded as claim data for P4P program. It was later analyzed retrospectively.
History of diabetic microvascular complications (retinopathy, neuropathy, and nephropathy) and macrovascular complication (coronary artery disease (CAD), stroke, and peripheral arterial disease (PAD)) were obtained. Definitions of the complications are listed in Table 1.
| Complication | Diagnosis/Definitions |
|---|---|
| Microvascular complications | |
| Diabetic retinopathy | Diagnose by fundoscopy |
| Diabetic neuropathy: | Diagnose by vibration perception threshold, Semmes-Weinstein monofilament, or nerve conduction velocity |
| Diabetic kidney disease (DKD) | Patients with an eGFR <60 ml/min/1.73 m2 or an urine albumin-creatinine ratio (UACR) ≧ 30 mg/g creatinine in the last urinary analysis within the past year. Positive UACR excludes infection or contamination |
| Macrovascular complication | |
| Coronary artery disease (CAD) | History of stable angina, acute coronary syndrome (ACS) or diagnose via coronary angiography |
| Stroke | History of ischemic stroke or transient ischemic attack (TIA), excluding traumatic brain injury and intracranial hemorrhage caused by brain tumor |
| Peripheral arterial disease (PAD) | History of amputation |
HbA1c level in the past 6 months; LDL-C level in the past year.
Statistical analysis
The proportion of patients attaining HbA1c < 7%, BP < 130/80 mmHg, LDL-C < 2.59 mmol/L or attainment of all three ABC targets constitutes quality of care.
The baseline characteristics, attainment of management goals, presence of complications and prescription patterns of antidiabetic agents were compared to patients with and without DKD by Students’ T-test for continuous variables and Fisher’s exact test for categorical variables.
The odds ratio (OR) of macrovascular complications, attainment of individual’s goals, and attainment of ABC goals in patients with and without DKD was calculated by logistic regression. Patients’ complications were unadjusted and patients’ goal attainment was adjusted by age, sex, body mass index (BMI) and diabetes duration. The OR of antidiabetic medications among DKD patients were adjusted based on baseline characteristics (age, sex, BMI, diabetes duration) and HbA1c. All statistical analyses were conducted with R version 4.0.0. P < 0.05 was considered statistically significant.
Results
Baseline characteristics
A total of 7,200 type 2 DM patients were enrolled in this study, baseline characteristics shown in Table 2: 49.6% male, mean age 62.56 ± 11.99 years old, diabetes duration of 8.67 ± 6.79 years and generally overweight (mean BMI 26.49 ± 4.41 kg/m2). DM complications among enrolled patients included 7.1% with CAD and 2.3% with documented cerebrovascular events. In addition, 20.96% were with retinopathy, 13.53% with neuropathy, and 44% with DKD. Mean eGFR is 79.46 ± 26.33 ml/min/1.73 m2.
| Total (n = 7200) | DKD (n = 3168) | Non-DKD (n = 4032) | p | ||
|---|---|---|---|---|---|
| Age (years) | 62.56 ± 11.99 | 65.15 ± 12.10 | 60.52 ± 11.51 | <0.001 | |
| Sex | Male (%) | 49.61 | 49.02 | 50.07 | 0.38 |
| Female (%) | 50.39 | 50.98 | 49.93 | ||
| Diabetes duration (years) | 8.67 ± 6.79 | 10.31 ± 7.49 | 7.38 ± 5.88 | <0.001 | |
| BMI (kg/m2) | 26.49 ± 4.41 | 26.61 ± 4.38 | 26.39 ± 4.43 | 0.04 | |
| eGFR (ml/min/1.73m2) | 79.46 ± 26.33 | 66.10 ± 27.60 | 89.96 ± 19.72 | <0.001 | |
| HbA1c (%) | 7.22 ± 1.36 | 7.38 ± 1.48 | 7.10 ± 1.25 | <0.001 | |
| Medication profile | |||||
| Average number of antidiabetic agents | 2.42 ± 1.16 | 2.55 ± 1.16 | 2.32 ± 1.15 | <0.001 | |
| Treatment combination | No therapy (%) | 2.35 | 2.15 | 2.50 | <0.001 |
| Monotherapy (%) | 22.00 | 17.93 | 25.20 | ||
| Dual therapy (%) | 28.49 | 27.78 | 29.04 | ||
| Triple therapy (%) | 29.22 | 31.50 | 27.43 | ||
| Quadruple and more therapy (%) | 17.94 | 20.64 | 15.82 | ||
| Patients on insulin therapy (%) | 21.64 ± 41.18 | 28.50 ± 45.15 | 16.25 ± 36.89 | <0.001 | |
Patients with DKD were generally older and has had longer diabetes duration. Their HbA1c level was significantly higher and were at higher comorbidity risk for hypertension yet not dyslipidemia. The average number in classes of antidiabetic agents prescribed and percentage of patients on insulin therapy were both higher among DKD patients, predictable among advanced diabetes patients.
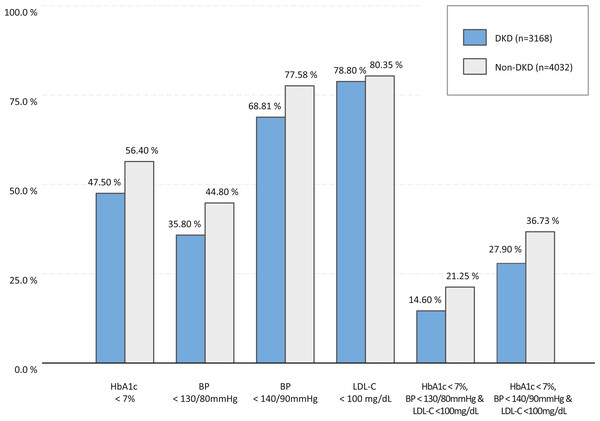
Attainment of treatment goals and complications
Overall, enrolled DM patients had a mean HbA1c of 7.22 ± 1.36%, a mean LDL-C 2.09 mmol/L, a mean systolic blood pressure (SBP) 129.75 ± 15.16 mmHg and a mean diastolic blood pressure (DBP) 74.75 ± 10.27 mmHg. Percentage of ABC goal attainment was 52.5% in HbA1c < 7%, 40.9% in BP < 130/80 mmHg, and 79.7% in LDL-C < 2.59 mmol/L. 18.3% of the enrolled patients achieved all three ABC goals, while less DKD patients attained the goal for HbA1c (47.5% vs. 56.4%, p < 0.001), BP (35.8% vs. 44.8%, p < 0.001), and ABC (14.6% vs. 21.25%, p < 0.001) (Fig. 1).
Figure 1: The percentages of patients attaining ABC goals.
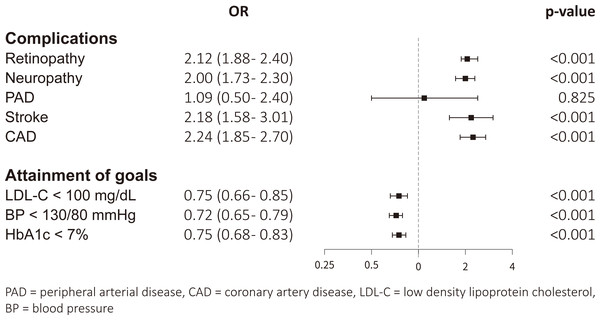
Retinopathy and neuropathy occurred in 28.00% and 18.14% of these DKD patients. The prevalence of PAD, stroke and CAD were 0.38%, 3.35% and 10.01%, respectively. After adjustment for multivariable regression, DKD patients were less likely to attain HbA1c, BP, and LDL-C goals and were more likely to experience microvascular and macrovascular diseases (Fig. 2).
Figure 2: Adjusted odds ratio of complications among DM patients with and without DKD.
Gender difference of DKD patients
The prevalence of CKD in male and female were 43.2% and 44.5%, respectively. Among DKD patients, male patients are more likely to have CAD (11.7% vs. 8.4%, p = 0.003) and proteinuria (82.7% vs. 77.1%, p < 0.001), but overall eGFR was higher (67.4 vs. 64.8 ml/min/1.73 m2). The prevalence of PAD, stroke, retinopathy, and neuropathy were similar between different genders.
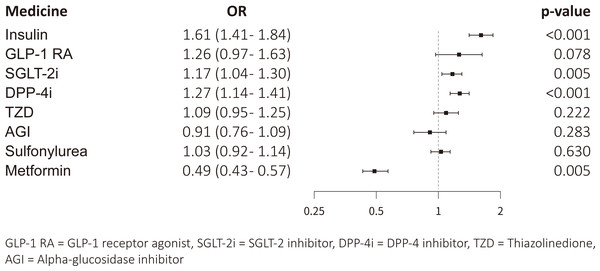
Prescription pattern
After adjustment, DKD patients were more likely to receive DPP-4 inhibitors (OR 1.27, 95% CI [1.14–1.41], p < 0.001), SGLT-2 inhibitors (OR 1.17, 95% CI [1.04–1.30], p = 0.005), and insulin therapy (OR 1.61, 95% CI [1.41–1.84], p < 0.001) than those without DKD. Metformin was less frequently prescribed among DKD patients. (OR 0.49, 95% CI [0.43–0.57], p < 0.001) (Fig. 3).
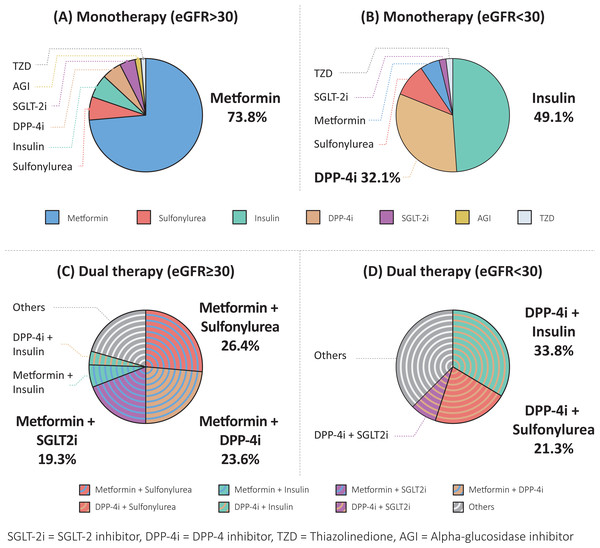
Stratified by different treatment regimens and eGFR status, Fig. 4 shows the percentage of each class of antidiabetic agent prescribed. Among patients with eGFR ≥ 30 ml/min/1.73 m2 on monotherapy, metformin was most frequently prescribed (73.8%) followed by sulfonylurea (6.6%) and then insulin (6.6%). Among patients with eGFR <30 ml/min/1.73 m2 on monotherapy, nearly half were prescribed insulin followed by DPP-4 inhibitors.
Figure 3: Adjusted odds ratio of individual classes of prescribed antidiabetic agents among patients with and without DKD.
Figure 4: The combinations and proportions of antidiabetic agents prescribed in different treatment regimens and eGFR stages.
(A) Monotherapy in eGFR ≥30 ml/min/1.73 m2, (B) monotherapy in eGFR <30 ml/min/1.73 m2, (C) dual therapy in eGFR ≥30 ml/min/1.73 m2 and (D) dual therapy in eGFR <30 ml/min/1.73 m2.Patients on dual therapy with eGFR ≥ 30ml/min/1.73m2, metformin-based combination was the most common regimen. The most common combinations were metformin with sulfonylurea (26.4%), metformin with DPP-4 inhibitors (23.6%) and then metformin with SGLT-2 inhibitors (19.3%). 30% dual therapy patients received other combinations in the order of DPP-4 inhibitors with sulfonylurea (3.5%), metformin with thiazolidinedione (3.0%) and SGLT-2 inhibitors with sulfonylurea (3.0%). Lastly, among dual therapy patients with eGFR < 30 ml/min/1.73 m2, their regimen was characterized by DPP-4 inhibitor-based medications. Insulins is frequently prescribed among eGFR < 30 ml/min/1.73 m2 patients.
Discussion
To our knowledge, this was the first large-scale primary diabetes care study initiated by local clinics on diabetes goal attainment, complications, and prescription patterns of DKD patients in Taiwan. The results not only revealed real-world practice outcomes, it but also revealed the unmet needs of DKD care at the primary care level.
DKD is the major cause for ESRD globally and attributes to multiple cardiovascular related morbidities. Numerous studies in the past had been conducted to determine the effectiveness of intensive intervention to improve outcomes of DM patients with DKD. First, intensive glycemic control to attain goals of HbA1c < 6.5% or fasting glucose of < 6 mmol/L was shown in multiple clinical trials to slow the decline of eGFR and progression of proteinuria (Ismail-Beigi et al., 2010; Patel et al., 2008; UK Prospective Diabetes Study Group, 1998a; UK Prospective Diabetes Study Group, 1998b; Zoungas et al., 2014). Second, strict control of SBP was shown to reduce mortality and proteinuria in type 2 diabetes (Accord Study Group et al., 2010; Emdin et al., 2015; UK Prospective Diabetes Study Group, 1998c). Treatment with angiotensin converting enzyme inhibitors (ACEIs) or angiotensin II receptor blockers (ARBs) decreases progression to ESRD (Brenner et al., 2001; Lewis et al., 1993; Lewis et al., 2001). As for LDL-C management, 160 type 2 DM patients with persistent microalbuminuria were enrolled in the STENO-2 Study, they were randomly assigned to receive either intensive (experiment group) or conventional therapy (control group). The experimental group had targets of attaining HbA1c < 6.5%, fasting total cholesterol < 4.53 mmol/L, fasting serum triglyceride (TG) < 1.69 mg/dL and BP < 130/80 mmHg. Compared to the conventional therapy group, the intensive therapy group had a lower risk of cardiovascular related deaths, cerebrovascular events, and progression to ESRD; confirming the cardio- and reno-protective effects of multifactorial control (Gaede et al., 2008). In our study, DKD patients represented the population with advanced DM complications compared to DM non-DKD patients; DKD patients has had longer diabetes duration since diagnosis (10.3 years vs. 7.4 years), higher HbA1c levels (7.4% vs. 7.1%), and were prescribed more categories of antidiabetic agents than non-DKD DM patients. A significantly higher rate of micro- and macrovascular complications was observed among DKD patients. The percentage of attaining either individual HbA1c, BP, LDL-C goal or attainment of all three ABC goals were all lower among DKD patients. Although insulin resistance and beta cell exhaustion may be of challenge for glycemic management in the later years of diabetes progression, we do not find poor LDL-C control directly associated with DM etiology. Thus, stricter LDL-C management should be emphasized for better DKD management in the future.
The importance of attaining ABC goals is widely advocated across different guidelines in diabetes care. In the USA, the National Health and Nutrition Examination Survey (NHANES) shows better diabetes management in attaining all three ABC goals from 2.7% in 1988–1994 to 12.2% in 1999–2006, and 25.9% in 2007–2010. Yet, compliance dropped to 20.7% between 2011-2014 possibly due to the adaptation of a less stringent goal set for frail DM patients (Cheung et al., 2009; Cowie, 2019; Saydah, Fradkin & Cowie, 2004). In Taiwan, comparing our study to a prior study conducted in 2006; we, too, find diabetes management improved over the years. In the 2006 study, 4.5% DM patients achieved all ABC goals and 30–35% attained individual goals (Yu et al., 2009). In our study, 18.3% DM patients achieved all ABC goals, 52.5% attained HbA1c, 40.9% attained BP and 79.7% attained their LDL-C goal.
The improvements may be due to the effective primary care at local clinics. In our study, all primary care clinics were registered under the Diabetes Share Care Network in Taiwan, a P4P program shown to provide better outcomes for diabetes patients. Lee et al. points out that participants of the P4P program had a significantly lower all-cause, diabetes-, and cancer-related mortality in each analytic year between 2005 to 2014. Meanwhile, frequency of diabetes-related hospitalization and emergency department visits were also lower. Over the years, due to our National Health Insurance (NHI) service fee reimbursement policy for lab and eye examinations, utilization of nephro- and retinopathy screening rose and detection of nephro- and retinopathy among diabetes grew (Lee et al., 2019). In our cohort study, most DKD patients were detected at either routine examination or by urinary examination.
For the past 20 years, the percentage of diabetes goal attainment kept improving. As routine diabetes health education is reimbursed with additional bonus to patients attaining the goal of HbA1c and LDL-C, diabetes health education attendance increased and dietitian-led interventions proved to provide better glycemic control under P4P (Sung et al., 2011). As for medication treatment, diabetes patients in our study utilized more classes of antidiabetic medications compared to the 2005-2014 cohort study, indicating a more aggressive medication intervention (Chu et al., 2019). Overall, the Share Care Network provided better self-management support, complication detection, and enabled goal-oriented treatments that contributed to better diabetes management and control.
Our data revealed that male DKD patients are associated with higher prevalence of CAD and proteinuria, but also higher eGFR. This is compatible with the observation with other studies, which pointed out that men DM men are at higher risk for albuminuric phenotype, whereas women are at higher risk for eGFR impairment. The observations are not conclusive and require more study to confirm (Giandalia et al., 2021).
Because of the cardio- and reno-protective effects, SGLT-2 inhibitors and GLP-1 RAs have been recommended to diabetes patients with ASCVD, heart failure or CKD (American Diabetes Association Professional Practice et al., 2022). Several large-scale randomized controlled trials have proved SGLT-2 inhibitors improve renal composite outcomes, slow eGFR decline and decrease albuminuria (Bailey, Day & Bellary, 2022). The reno-protective effect is now considered independent of glucose lowering effect. GLP-1 RAs reduce albuminuria, but the efficacy on hard renal endpoint remained equivocal (Greco et al., 2019). The Taiwan Society of Cardiology published a consensus on the pharmacological management of patients with type 2 diabetes and cardiovascular diseases in 2020 that diabetes patients with stage 3 CKD, an SGLT-2 inhibitor in combination with metformin is the only recommended regimen in dual therapy (Chiang et al., 2020). However, in our survey, only 19% (152/798) of diabetes patients received the combination of an SGLT-2 inhibitor with metformin, in contrast to 23.3% (186/798) on DPP-4 inhibitor with metformin and 26% (208/798) on sulfonylurea with metformin. This finding shows a relatively low prescription rate of SGLT-2 inhibitors and GLP-1 RAs among DKD patients. Similar to our results, the multinational study on cardiovascular disease pointed out that an SGLT2i and GLP-1 RA were prescribed in only 16.0% and 10.1% of type 2 DM patients (Mosenzon et al., 2021).
In our study, DKD patients were more frequently prescribed with insulin and DPP-4 inhibitors, but less likely to be prescribed with metformin. As DKD patients are often older, with lower eGFR, and higher HbA1c, DPP-4 shows a safer profile among aged and renal impaired patients. In addition, insulin was more frequently prescribed due to poor glycemic control and limited medication choices among diabetes patients with lower eGFR. Diabetes patients with or without DKD had similar chances of receiving sulfonylureas. In our study, maybe due to a relatively loose NHI reimbursement criteria and clinical inertia, sulfonylurea is the most prescribed second line medication in combination with metformin among DKD patients. despite its increased risk for hypoglycemia in patients with impaired renal function. Although being prohibited, it is observed that 5.7% DKD patients with eGFR < 30 ml/min/1.73 m2 received off-label metformin. Finally, our analysis finds that among DKD patients with HbA1c > 7%, 18.1% were on monotherapy, 38.3% on dual therapy, and 58.1% on triple therapy. More aggressive glycemic control should be followed by DKD patients not attaining recommended goals.
Our study has several limitations. First, in this observational, cross-sectional study, causal inferences cannot be performed due to limited temporal data. Second, as the dosage data of each oral antidiabetic agent (OAD) cannot be obtained, we used the categories of OAD as an indicator of the level of difficulty in controlling diabetes; we are aware, different stages of medication combinations and dosages may confound our outcome. Third, as the data were obtained from 43 primary clinics without a well-established electronic health record system or care management system, comorbidities and complications requiring advanced detection equipment, prevalence of complications (such as PAD), retinopathy, and neuropathy may be underestimated. Sampling bias may be minimized because the patients were selected randomly according to the visiting days in the study interval.
Conclusions
In conclusion, diabetes patients in Taiwan receive a generally satisfactory diabetes primary care at local clinics. However, we suggest more aggressive HbA1c, blood pressure, and LDL-C management among DKD patients to prevent micro- and macrovascular complications. Prescription of SGLT-2 inhibitors and GLP-1 RAs are frontline therapy medications under-prescribed probably due to reimbursement criteria or patients’ and physicians’ choice. Further investigation and analysis are required.
Supplemental Information
Raw data
All patient’s baseline characteristics, physical examination, laboratory examinations, presence of complications and antidiabetic agents prescribed. The data was used to investigate the quality of care and prescription patterns of patients with DKD receiving primary care at local clinics in Taiwan.