Cuffless blood pressure estimation based on haemodynamic principles: progress towards mobile healthcare
- Published
- Accepted
- Received
- Academic Editor
- Shawn Gomez
- Subject Areas
- Bioengineering, Cardiology, Drugs and Devices, Global Health, Human-Computer Interaction
- Keywords
- Blood pressure, Haemodynamic principle, Modified normalized pulse volume, Smartphone, Hypertension, Mobile health, Cuffless, Heart disease, Healthcare, Smart
- Copyright
- © 2021 Yamakoshi et al.
- Licence
- This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, reproduction and adaptation in any medium and for any purpose provided that it is properly attributed. For attribution, the original author(s), title, publication source (PeerJ) and either DOI or URL of the article must be cited.
- Cite this article
- 2021. Cuffless blood pressure estimation based on haemodynamic principles: progress towards mobile healthcare. PeerJ 9:e11479 https://doi.org/10.7717/peerj.11479
Abstract
Background
Although cuff-sphygmomanometry is used worldwide in medical and healthcare fields, it is a fact that the use of an occlusive cuff to obtain blood pressure (BP) is troublesome and inconvenient. There have therefore been on-going efforts to devise methods that do not require the use of a cuff, almost all being based on the measurement of pulse wave velocity or pulse transit time, but so far few significant developments have been made, especially regarding measurement accuracy. We have previously reported a smartphone-based cuffless method using a linear multiple regression calibration model comprising of BP obtained with a cuff-sphygmomanometer as an objective variable and modified normalized pulse volume (mNPV: a measure of vasoconstrictive activity in a finger) and pulse rate (PR) as explanatory variables. This requires a number of subjects to construct a calibration model and thus is largely dependent on the accuracy due to the model. To address these drawbacks, we report here a new cuffless method to surpass considerably the results of our previous study as well as earlier works.
Methods
With this method we can estimate BP, with much higher accuracy, using mNPV and PR, both also obtained from a smartphone-derived photoplethysmogram. The subject firstly performs a cuff-based BP measurement in parallel with the acquisition of mNPV and PR from a smartphone. These parameters are set as initial values (BPc0, mNPV0 and PR0; initial calibration procedure). Then, the estimated BP (BPe) can be calculated from the relation: “BPe = (BPc0·PR·mNPV)/(PR0·mNPV0)”, which is derived from the so-called haemodynamic Ohm’s law. To validate this method, preliminary experiments using 13 volunteers were carried out to compare results from the new method with those from the cuff-sphygmomanometry, used as a reference.
Results
Altogether 299 paired data sets were analyzed: A good agreement was found between the cuff-based and the estimated BP values, with correlation coefficients of 0.968 for systolic BP (SBP), 0.934 for mean BP (MBP) and 0.844 for diastolic BP (DBP). Bland-Altman analyses for the BPe (SBPe, MBPe, DBPe) and the BPc (SBPc, MBPc, DBPc) values also supported these comparison results. Mean absolute differences between the BPe and the BPc values in total subjects were less than 5 mmHg. Fairly good tracking availability in terms of time series data of the BPc against the corresponding BPe values was also confirmed in each subject during the study periods (1–2 weeks for 12 subjects and about 4 months for one subject).
Discussion
The present study reported the successful development of the new cuffless BP estimation method, given as the status of a trial stage of investigation. This method could easily be used with various smartphones, smart watches, and finger-based devices, and it appears to have significant potential as a convenient substitute for conventional cuff-sphygmomanometers as well as for practical application to mobile healthcare.
Introduction
It is well known that high arterial blood pressure (BP) is associated with increased risk of disease and mortality (James et al., 2014; Poulter, Prabhakaran & Caulfield, 2015). However, because BP can fluctuate by a significant amount (Parati et al., 2013) both on a beat-by-beat basis and in the long-term, it is important that it is checked frequently, especially in the case of the hypertensive subject. Non-invasive methods for checking beat-by-beat or intermittently obtained BP are preferred, and several are currently available, such as variations of the well-known Riva-Rocci mercury sphygmomanometer, as well as volume oscillometry (Yamakoshi et al., 1982; Parati et al., 2013; Yamakoshi et al., 2014), volume compensation (Yamakoshi, Shimazu & Togawa, 1980; Matsumura et al., 2017) and tonometry (Hansen & Staber, 2006).
During the use of conventional sphygmomanometry, an occlusive cuff must be applied to a finger, wrist, or the upper arm, and cuff pressure must be controlled to determine BP values. Despite their widespread use almost every minute of every day by tens of millions of people across the globe, arm-cuff-based BP measurement technologies in particular are still often considered to be inconvenient and cumbersome due to their reliance on the inflatable cuff. There have therefore been on-going efforts over recent decades to devise methods that do not require the use of the cuff.
The phrase “cuffless BP” is now a generic term for methods that determine BP without the use of a cuff. These approaches seek to avoid the discomfort or inconvenience associated with cuff inflation/deflation and also to obviate the need for a means of cuff pressurisation, which, in addition, increases the cost and complexity of the technology as well as complicating the measurement process. Almost all cuffless BP estimation methods proposed to date have been based on the measurement of pulse wave velocity (PWV) or pulse transit time (PTT) using various relationships between cuff-based BP and PWV or PTT (Payne et al., 2006; Gesche et al., 2012; Mukkamala et al., 2015; Sharma et al., 2017; Ding et al., 2017; Nabeel, Jayaraj & Mohanasankar, 2017).
In contrast to this, our group recently developed a much simpler method for cuffless BP estimation (Matsumura et al., 2018) based on a linear multiple regression model. Briefly, in this method, pulse rate (PR) and a modified normalized pulse volume (mNPV) (Lee et al., 2013) are used as explanatory variables, both of which can be obtained from the smartphone-derived reflectance-mode photoplethysmogram (PPG) (Matsumura & Yamakoshi, 2013; Lee et al., 2013). A linear multiple regression (calibration) analysis was made using the objective variable (BP; systolic (SBP), mean (MBP and diastolic BP (DBP) in each) measured by a cuff-based sphygmomanometer and the explanatory variables (PR and mNPV), to construct a BP calibration (regression) equation using a number of subjects. Then, the estimated BP can be calculated by the calibration equation, using PR and mNPV variables acquired by a smartphone (Matsumura & Yamakoshi, 2013).
The mNPV can be calculated from the amplitude of the pulsatile component (PPGAC) superimposed on the PPG signal, divided by the mean DC component (PPGDC) (i.e., mNPV = PPGAC/PPGDC). This is an alternate variable of NPV obtained with a transmittance-mode PPG, which was found to be almost equivalent and was originally proposed as a valid measure to represent vascular tone or sympathetic arteriola constrictive activity in a finger (Sawada, Tanaka & Yamakoshi, 2001).
It is clear that the accuracy of the estimated BP values by this method must largely be dependent on the magnitude of the variance in the regression, or in other words, on the accuracy of the BP calibration equation employed. This, in turn, means that the number of subjects used to determine the regression equation could greatly influence the estimated accuracy and error.
In order to avoid such erroneous factors in the regression and error analysis, we devised a new, more straightforward, cuffless technique so as to firstly pre-set cuff-based BP together with the PR and mNPV variables as initial values within an individual person. That person can then obtain the estimated SBP, MBP and DBP values using only PR and mNPV variables. In this study, we also used a smartphone (iPhone) to obtain the PR and mNPV variables. With this broad background, the objective of the present study was to validate this new technique through preliminary experiments to compare results from the new method with those obtained from a cuff-based sphygmomanometer as a reference method.
Materials & methods
Principle of BP estimation
The principle of BP estimation in this study is based on the well-known haemodynamic Ohm’s law, to be given as:
(1) with the proviso that central venous pressure can be considered to be negligibly small as compared to MBP (Guyton & Hall, 1996). It has been reported that under resting conditions CO and TPR are essentially correlated with PR and mNPV, respectively (Obrist et al., 1978; Chau et al., 1978; Light, 1981; Sherwood, Dolan & Light, 1990; Sawada, Tanaka & Yamakoshi, 2001; Protogerou et al., 2007), and thus taking into consideration these evidential findings, we can reasonably assume that CO is approximately proportional to PR (CO ≒ (constant k1) × PR) and TPR is also approximately expressed as TPR ≒ (constant k2) × mNPV. A caveat is that this applies to the case of a subject who performs BP measurement under resting conditions, except for the case where they are carrying out any kind of exercise. Then, by making substitutions in Eq. (1) for CO and TPR we have:
(2)
Now, the subject is firstly requested to measure his/her own SBP/DBP using a cuff-based sphygmomanometer in parallel with the use of their smartphone to acquire PR and mNPV variables, pre-setting these variables SBPc0/DBPc0, PR0 and mNPV0 as initial values. This is the initial calibration (or setting) procedure. The subscript ‘c’ indicates the BP values determined by the cuff sphygmomanometer. We can calculate MBPc from the following formula: MBPc = DBPc + (SBPc − DBPc)/3. The following equation, therefore, holds, using initial values as,
(3)
Diving Eq. (2) by Eq. (3), we get the following equation, with the constants now eliminated, as:
(4)
In this equation, MBPc0 (as well as SBP c0 and DBP c0) is obtained through the use of the cuff sphygmomanometer and thus is different from the quantity of MBP (SBP and DBP as well), being considered and termed as an estimated MBP (MBPe: also termed as SBPe and DBPe). Equation (4) is therefore rewritten as the following simple equation:
(5)
Similarly, tentatively assuming that the same relationship holds with respect to SBPe and DBPe, we can obtain the following equations as:
(6)
(7)
If either SBPe or DBPe is obtained by Eqs. (6) or (7), either one can also be simply calculated together with MBPe as follows:
(6’)
(7’)
These equations mean that BPe (SBPe/MBPe/DBPe) values can be estimated when the initial calibration procedure is done to determine BPc0 (SBPc0/MBPc0/DBPc0) along with PR0 and mNPV0. In other words, considering that mNPV corresponds to peripheral resistance, BP is to be linearly related to “rate resistance-index product” (PR × mNPV).
Participants and ethical statements
A total of 13 volunteers (six males and seven females) participated in this study. All were Japanese, 19 to 73 years old, living their normal daily life in Tokyo, Kobe, and Sapporo cities. A total of 4 of the 13 subjects (No. 8, No. 11, No. 12 and No. 13 in Table 1) have suffered from grade 1 hypertension and have been taking antihypertensive agents every day. The others, 19 to 53 years old, had no current cardiovascular disease and did not take any prescription medications, although 2 subjects (No. 1 and 2), who have been living a normal daily life, appeared to have hypotension.
| Sub. no. | Gender | Age | BMI [kg/m2] | Number of measurements (measurement periods) | Mean (S.D.) brachial BP [mmHg] and PR [bpm] values | Mean (S.D.) PR [bpm] and mNPV [a.u × 10−2.], and estimated BP [mmHg] values | Mean absolute difference MAD (S.D.) [mmHg] | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| SBPC <initial value> | MBPC<initial value> | DBPC<initial value> | PRC | PR <initial value: PR0> | PR/PR0 | mNPV <initial value: mNPV0> | mNPV/mNPV0 | SBPe (SBPe*) | MBPe | DBPe (DBPe*) | MAD of SBPc & SBPe(SBPe*) | MAD of MBPC & MBPe | MAD of DBPC & DBPe(DBPe*) | |||||
| 1 | Female | 19 | 22.7 | 19 (14 days) | 110 (6.3) <113> | 80 (3.9) <81> | 66 (3.0) <65> | 80.7 (7.87) | 80.8 (8.83) <76.8> | 1.05 (0.118) | 5.87 (1.78) <4.16> | 1.41 (0.428) | 107 (6.0) (110 (6.2)) | 84 (4.7) | 71 (4.0) (73 (4.1)) | 3.8 (2.3) (2.4 (1.6) | 3.9 (1.6) | 5.8 (1.6) (7.3 (2.2)) |
| 2 | Female | 21 | 22.6 | 19 (12 days) | 104 (3.7) <111> | 81 (4.1) <85> | 69 (5.0) <72> | 58.7 (5.63) | 58.6 (4.59) <66.2> | 0.88 (0.071) | 3.52 (1.23) <4.04> | 0.87 (0.306) | 103 (5.2) (103 (5.2)) | 79 (4.0) | 67 (3.4) (67 (3.4)) | 2.9 (1.9) (2.9 (1.9)) | 2.0 (1.9) | 3.1 (2.2) (3.1 (2.2)) |
| 3 | Male | 38 | 23.2 | 20 (14 days) | 138 (7.3) <116> | 103 (5.1) <90> | 86 (4.4) <77> | 66.5 (5.64) | 67.2 (6.28) <52> | 1.29 (0.124) | 2.28 (1.01) <1.47> | 1.55 (0.688) | 136 (8.3) (136 (8.3)) | 106 (6.4) | 91 (5.5) (91 (5.5)) | 4.3 (2.0) (4.3 (2.0)) | 3.3 (2.6) | 4.8 (3.0) (4.8 (3.0)) |
| 4 | Female | 39 | 19.4 | 20 (12 days) | 111 (3.5) <112> | 85 (3.4) <86.7> | 72 (4.4) <74> | 71.3 (6.17) | 72.1 (4.64) <72.6> | 0.99 (0.066) | 3.78 (1.18) <3.80> | 0.99 (0.311) | 112 (5.5) (112 (5.5)) | 87 (4.3) | 74 (3.6) (74 (3.6)) | 4.2 (2.9) (4.2 (2.9)) | 3.9 (2.0) | 4.1 (3.0) (4.1 (3.0)) |
| 5 | Female | 45 | 20 | 20 (11 days) | 103 (5.9) <95> | 71 (4.4) <65.7> | 56 (4.1) <51> | 69.1 (5.73) | 68.3 (5.36) <71.1> | 0.96 (0.078) | 2.45 (0.656) <3.76> | 0.65 (0.174) | 104 (5.7) (104 (5.8)) | 72 (4.0) | 56 (3.1) (56 (3.1)) | 2.8 (1.8) (2.8 (1.9)) | 1.8 (1.3) | 1.9 (1.6) (1.9 (1.6)) |
| 6 | Male | 46 | 21.9 | 18 (19 days) | 124 (7.6) <125> | 92 (5.1) <90> | 76 (4.8) <72> | 66.1 (4.67) | 68.3 (2.90) | 0.94 (0.041) | 4.10 (1.02) <4.42> | 0.93 (0.233) | 120 (7.1) (120 (7.1)) | 86 (5.1) | 69 (4.1) (69 (4.3)) | 3.7 (2.0) (3.6 (2.0) | 5.6 (2.8) | 7.1 (3.1) (7.1 (3.1)) |
| 7 | Female | 53 | 23.1 | 20 (12 days) | 105 (6.4) <110> | 78 (5.0) <82> | 64 (5.3) <68> | 55.9 (3.57) | 56.3 (3.33) <49> | 1.15 (0.074) | 6.22 (1.76) <3.40> | 1.82 (0.515) | 105 (6.9) (105 (6.9) | 78 (5.1) | 65 (4.3) (65 (4.3)) | 3.6 (2.1) (3.6 (2.1)) | 2.4 (1.5) | 3.1 (2.3) (3.1 (2.3)) |
| 8HY | Male | 67 | 24.9 | 19 (10 days) | 139 (7.6) <142> | 98 (4.7) <99.3> | 77 (4.4) <78> | 70.4 (3.57) | 70.1 (3.64) <65.7> | 1.07 (0.057) | 7.52 (2.00) <5.90> | 1.27 ((0.339) | 140 (10.1) (140 (10.1)) | 98 (7.1) | 77 (5.5) (77 (5.5-)) | 4.7 (2.5) (4.7 (2.5)) | 3.2 (2.1) | 3.7 (2.4) (3.7 (2.4)) |
| 9 | Male | 67 | 27.3 | 19 (5 days) | 125 (10.2) <118> | 91 (6.2) <88> | 74 (5.0) <73> | 64.7 (5.10) | 63.8 (3.65) <62.3> | 1.02 (0.060) | 8.48 (2.38) <9.16> | 0.93 (0.259) | 126 (10.2) (126 (10.2)) | 94 (7.6) | 78 (6.3) (78 (6.3)) | 2.8 (1.7) (2.8 (1.7)) | 3.9 (2.4) | 5.3 (3.3) (5.3 (3.3)) |
| 10 | Female | 71 | 20.6 | 17 (12 days) | 121 (6.2) <117> | 90 (4.6) <87> | 75 (4.5) <72> | 70.2 (4.25) | 70.4 (4.77) <72.0> | 0.98 (0.068) | 7.51 (2.25) <5.45> | 1.37 (0.413) | 121 (7.3) (121 (7.3)) | 90 (5.4) | 75 (4.5) (75 (4.5)) | 3.5 (2.7) (3.5 (2.8)) | 3.6 (2.1) | 3.9 (2.4) (3.9 (2.4)) |
| 11HY | Male | 72 | 24.9 | 61 (119 days) | 138 (11.9) <134> <2nd: 128> <3rd: 128> | 99 (8.8) <95.3> <2nd: 93.3> <3rd:90> | 80 (8.0) <76> <2nd: 76> <3rd: 71> | 64.1 (5.19) | 64.1 (5.08) <68> <2nd: 72> <3rd: 67> | 0.97 (0.084) 2nd 0.84 (0.068) 3rd 0.96 (0.071) | 2.89 (1.35) <2.79> <2nd: 8.13> <3rd: 3.80> | 0.69 (0.239) 2nd 0.50 (0.260) 3rd 0.75 (0.284) | 138 (11.9) (138 (11.9)) | 98 (8.8) | 78 (7.3) (78 (7.3)) | 2.8 (2.0) (2.8 (2.0)) | 3.7 (2.7) | 5.0 (3.4) (5.0 (3.4) |
| 12HY | Female | 72 | 19.7 | 17 (6 days) | 120 (9.3) <115> | 86 (6.9) <84.3> | 69 (6.4) <69> | 68.1 (2.89) | 69.7 (4.12) <77.8> | 0.90 (0.055) | 5.17 (1.91) <7.14> | 0.73 (0.267) | 118 (10.7) (117 (10.6)) | 86 (7.8) | 71 (6.4) (70 (6.4)) | 4.1 (2.9) (4.1 (2.9)) | 2.3 (2.1) | 2.8 (2.7) (2.7 (2.7)) |
| 13HY | Male | 72 | 26.7 | 30 (14 days) | 136 (13.4) <139> | 97 (9.0) <98> | 78 (7.5) <78> | 65.1 (7.84) | 65.0 (7.17) <65.9> | 0.99 (0.11) | 4.79 (1.76) <8.05> | 0.60 (0.219) | 136 (12.1) (136 (12.3)) | 99 (9.5) | 81 (8.4) (80 (8.4)) | 3.3 (2.5) 3.1 (2.4) | 3.7 (2.3) | 5.1 (3.0) 5.1 (3.0) |
| Total | 3.5 (2.3) (3.3 (2.3)) | 3.4 (2.4) | 4.4 (3.1) (4.5 (3.2) | |||||||||||||||
Notes:
(a) superscript HY means hypertension with grade one, taking antihypertensive agents everyday.
(b) "Number of measurements" indicate the number excluded from the initial setting procedure in all subjects except that in the subject No. 11, in which the number is excluded from the initial setting and two times resetting procedures.
Written informed consent was obtained from all participants after we had provided them with a complete description of the study inclusive of measurement protocol and safety. This study was approved by the ethics committee of Showa University (Approval Reference Number: 2347) and conducted according to the principles expressed in the Declaration of Helsinki. This is not a replicated study.
Apparatus and measurements
All participants had their own smartphone, including iPhone 7, 8, X, XS, 11 and 11 Pro (Apple Inc., Cupertino, U.S.A.). An experimental app (named “Exp_app”) was provided for this study, a modified version of the iPhysioMeter app (Matsumura & Yamakoshi, 2013) previously designed by us, and installed in each participant’s iPhone.
The Exp_app was essentially the same as the iPhysioMeter app, the details of which were reported elsewhere (Matsumura & Yamakoshi, 2013). Briefly, this application was rewritten to be compatible with iPhone 7 and later devices using iOS 13.3 or subsequent upgrades (Apple Inc., Cupertino, U.S.A.). The program allows the iPhone to serve as a reflectance-mode photoplethysmograph (PPG), producing the PPG signal by employing the CMOS camera and LED light built into the iPhone as a photodetector and light source, respectively. The PPG signal was acquired from the subject’s left index fingertip with a sampling rate of 60 frames per second.
Both PR and mNPV (= PPGAC/PPGDC) data were obtained from the PPG signal on a beat-by-beat basis via an auto-analysis algorithm included in the iPhone software. Any values that were significantly different from those over the prior 5 s time span were assumed to be outliers. A significant difference was defined as one that increased the standard deviation (S.D.) values associated with PR and mNPV by more than 8.0 beats per minute (bpm) or 0.25 arbitrary units (a.u.), respectively (Bland & Altman, 1986; Matsumura et al., 2014).
A brachial cuff-sphygmomanometer (DSK-1051, NISSEI, authenticated by the European Society of Hypertension (ESH), Milan, Italy; Japan Precision Instruments Inc., Hachioji, Japan) was provided for each participant. BP measurements were made by this device to produce the reference values of SBPc and DBPc as well as the calculated MBPc (= DBPc + (SBPc – DBPc)/3).
All of these data, including the raw PPG signals, were stored in the iPhone of each participant who e-mailed the data after each measurement to one of the experimenters to combine with all data for analysis.
Measurement procedures
Experiments were carried out during normal daily life at each subject’s home, in a room temperature of around 24 to 26 °C, and humidity of around 45 to 55%. Throughout the measurements, the subject remained as motionless as possible, to sit for one min at rest in a chair with their left hand placed on a desk in front of them before starting the measurements; this was to reduce the appearance of movement artefacts. All of the subjects selected in this study knew very well how to operate the brachial cuff-sphygmomanometer provided, since they used their own sphygmomanometer routinely. It took about 40 s to obtain the brachial BP data and about 15 s to obtain the mean PR and mNPV values from averaging about 10 successive beat-by-beat data.
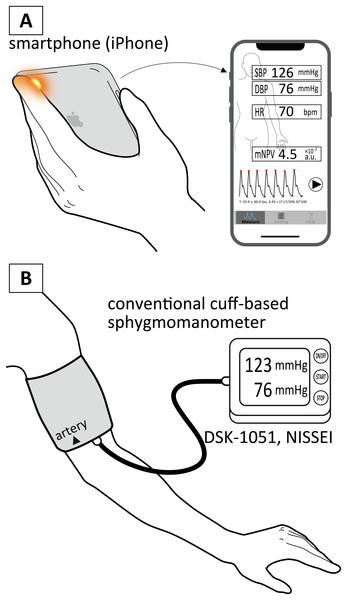
The participants were also asked to perform the BP measurements two or three times a day at any convenient time they wished. To make the contact condition between the iPhone CMOS camera and a subject’s fingertip almost the same, he/she was further reminded to place the iPhone softly on their left hand and keep their left index fingertip placed carefully over the camera, as shown in Fig. 1A. The fingertip was therefore just touching the camera. At this time, each subject was strongly recommended to mark their fingertip so as to place the camera almost in the exact same position for every measurement.
Figure 1: Illustrative drawings of measurement scenes.
Illustrative drawings of measurement scenes by a smartphone (iPhone) (A) and a conventional cuff-based sphygmomanometer (B).We have conducted preliminary experiments to measure simultaneously the contact pressure and PPG waveforms in this condition using a thin force sensor (FSR402, Interlink Electronics Inc., California, U.S.A.) fabricated into a donut shape. The pressure converted by the contact area was less than 2–3 mmHg, confirming that stable and reproducible PPG waveforms were obtained. Furthermore, the specially designed software (Exp_app) allowed the subject to watch their own PPG waveforms, as well as the calculated PR and mNPV values, on a beat-by-beat basis as displayed in the iPhone screen, in real time, during the measurement (also shown in Fig. 1A). If artifactual PPG waveforms, and/or unstable or outlying PR and mNPV values were observed, the subject stopped the procedure and then immediately restarted the measurement so as to minimize collection of erroneous data. This was also considerably helpful to reduce the appearance of movement artefacts and/or unstable PPG signals and for the subject to make a decision whether or not the signals were appropriate and/or acceptable.
After each BP measurement was made, the measurement by the iPhone continued to be carried out within about 30 s before major BP fluctuations occur, and then the subject manually input the obtained BP and pulse rate (PR) values (SBPc, DBPc and PRc) to the iPhone. Each subject was requested to carry out the first BP measurement twice or three times to ensure that they could obtain almost the same BP values, within about 5 mmHg. The mean BP values (SBPc0/DBPc0) and the iPhone measurement values (PR0/mNPV0) were set as initial values (i.e., this is the initial calibration procedure), being used for the calculation of BP estimation thereafter. The initial calibration procedure was made only once unless there was a considerable difference (over 30 mmHg or more) between the cuff-based and the estimated BP values.
The overall study periods lasted for 1–2 weeks to anticipate collecting about 20 paired data sets in each subject, but they could stop the process at any time according to their circumstances. One subject (No. 11 in Table 1) of the 13 volunteers proposed doing prolonged measurements at their convenience for about 4 months and 61 data sets were subsequently obtained from this subject.
Data analysis
All of the data sent by e-mail were checked by observing the raw PPG signals as well as the obtained values of SBPc, DBPc, PRc, PR and mNPV in each subject. This was just to determine whether or not there were artefactual data and outliers, according to the criteria of standard deviation (S.D.) values of PR and mNPV. Actually, since the subject could watch their own PPG waveforms as well as calculated PR and mNPV values on a beat-by-beat basis displayed in the iPhone screen, as mentioned above, the data transmitted by e-mail from each subject were all essentially artifact-free and valid during the measurement period of 10 successive beat-by-beat data. The averaged PR and mNPV values were used for analyses. The initial setting values from the relevant subject (No. 1–10, No. 12 and No. 13) were also excluded from the data analyses. In subject No. 11 the initial setting and the second and the third resetting values were excluded. Altogether 299 paired data sets were finally obtained from the subjects.
Correlation analyses were made in each and in all of the subjects between the estimated BP (BPe) values (SBPe, MBPe and DBPe) and the brachial BP (BPc) values (SBPc, MBPc and DBPc) as the reference. Bland–Altman error analyses (Bland & Altman, 1986) for the BPe and the BPc values were also done in all of the subjects. Mean absolute difference (MAD) was further calculated for the evaluation of agreement between the BPe and the BPc values. A trend chart of the BPe and the BPc values obtained from one subject (No. 11 in Table 1) is presented to show BP tracking performance of this method for a longer period of time.
Data availability
The data that support the findings of this study are available in PeerJ.
Results
Regression analyses in each subject
A total of 299 paired data sets were acquired for analyses obtained from 13 volunteer subjects. Table 1 summarizes the mean and S.D. values for all variables based on data acquired throughout the measurement process in each subject, along with the values of mean absolute difference (MAD [mmHg]) between the brachial BP (SBPc/MBPc/DBPc) and the estimated BP data (SBPe/MBPe/DBPe). SBPe* and DBPe* data calculated by Eqs. (6’) and (7’) are also included in Table 1 for reference.
Agreement between estimated and cuff-based BP data
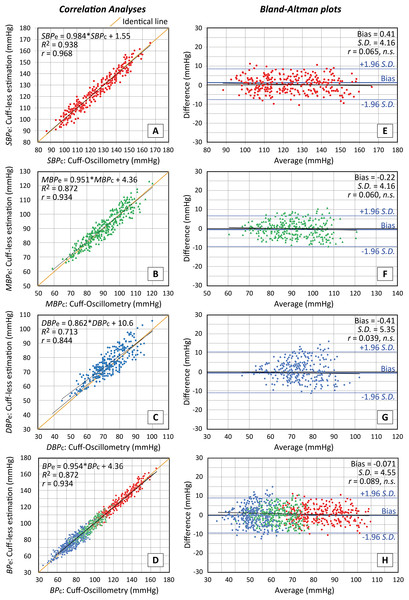
Figure 2 shows scatter plots in all subjects based on paired SBPe, MBPe and DBPe data calculated by Eqs. (5)–(7) using the PR and mNPV values acquired from the iPhone against corresponding brachial data (SBPc, MBPc and DBPc) determined by the cuff-based sphygmomanometer, along with the associated Bland–Altman plots. Such scatterplots using SBPe* and DBPe* were omitted since almost the same result as in Fig. 2 was obtained.
Figure 2: Accuracy of estimated values obtained with the proposed method.
Accuracy of estimated values obtained with the proposed method. Scatterplots of SBP (A), MAP (B), DBP(C) and total BP (including all of SBP, MBP and DBP) values (D) estimated using a smartphone against the values determined with a brachial cuff sphygmomanometer (n = 299 for SBP, MBP and DBP and n = 897 for total). Lines of identity (solid orange lines), regression lines (solid black lines) and regression formula together with the coefficient of determination R2 and the correlation coefficient r values are shown in each scatterplot. Corresponding Bland–Altman plots of SBP (E), MAP (F), DBP (G) and total BP values (H). Solid and dashed lines represent the fixed bias and the limits of agreement (bias ± 1.96 S.D.). (S.D.: standard deviation), respectively. Average = (brachial + estimate)/2, Difference = brachial − estimate. Pearson’s r values are also presented in each graph.Figures 2A–2D are the scatter plots respectively for SBPe vs SBPc, MBPe vs MBPc, DBPe vs DBPc and total BPe vs BPc, in which lines of identity (solid orange lines), regression lines (solid black lines) and regression formula together with the coefficient of determination R2 and the correlation coefficient r values are indicated. While Figs. 2E–2H are the Bland-Altman graphs in a similar manner to the above, in which fixed bias (M; drawn with solid lines) and S.D. values (limits of agreement of M ± 1.96 S.D.; drawn with dotted lines) together with Pearson’s r values, are presented.
MAD values between SBPc and SBPe (SBPe*), MBPc and MBPe, and DBPc and DBPe (DBPe*) were respectively 3.5 ± 2.35 (3.3 ± 2.32), 3.4 ± 2.41 and 4.4 ± 3.09 (4.5 ± 3.18).
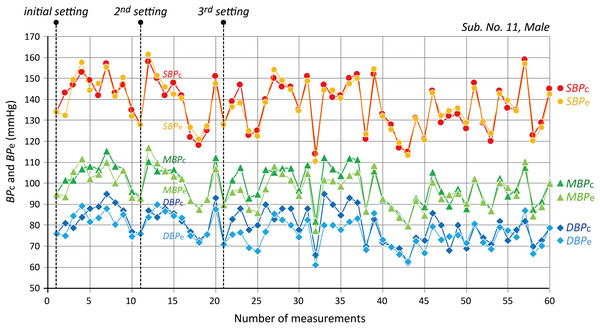
BP tracking availability
Fairly good tracking availability in terms of time series data of the BPc and PRc values by a cuff-sphygmomanometer against the corresponding BPe and PR values by an iPhone, was confirmed in each subject within 1–2 weeks of a study period. Figure 3 is an example of a trend chart of 61 data sets of SBPc/MBPc/DBPc and corresponding SBPe/MBPe/DBPe values obtained in one subject (No. 11) with a prolonged study period of about 4 months, showing good BP tracking availability.
Figure 3: An example of a trend chart.
An example of a trend chart of 61 data sets of SBPc/MBPc/DBPc and corresponding SBPe/MBPe/DBPe values obtained in one subject (No. 11) with the prolonged measurement period for about 4 months. See text for further explanation.Discussion
The goal of this work was to demonstrate a simple, suitably accurate, reliable for estimating BP without the use of an occlusive cuff. Although the present study constituted the status of a trial stage of development using a smartphone towards this goal, it is worth noting that estimated BP values by the new method described herein showed a good agreement with the measured values obtained by a cuff-based sphygmomanometer as a reference, provided that the subjects kept still, at rest, at home without any stressful tasks during the measurements. This means a limitation of this method at the present stage, thus indicating the need for a further study to be carried out under various measurement conditions. Therefore we discuss here advantages and disadvantages as well as technical improvements of this method, keeping such measurement limitation in mind.
It should firstly be noted that sequential measurements using the left hand were adopted as BP measurement by a brachial cuff-sphygmomanometer, followed immediately by a smartphone measurement, since subjects had to perform a series of measurement operations themselves which needed the use of their right hand. During the measurement, the subjects were requested to be at rest in a sitting position, so that any BP fluctuations could be considered to be acceptably small to enable the comparison analyses to be valid.
Taking also the real-life setting into consideration, in this study, all of the data were obtained from voluntary individuals during their normal daily life at home where they were exposed to little stress to cope by themselves, probably resulting in slight BP changes as compared to those in their normal away-from-home life. Actually, the BP variability in each subject was not so large, as inferred from the S.D. values shown in Table 1. It is also noted that the BP changes would be due mainly to the changes in the vascular-related variable mNPV rather than those in the cardiac-related variable PR, considering that the S.D. values of the ratio mNPV/mNPV0 were relatively large as compared to those of the ratio PR/PR0, as also shown in Table 1.
Under these measurement conditions during normal daily living, when plotted against BP values obtained using brachial sphygmomanometry as the reference (SBPc/MBPc/DBPc), SBPe, MBPe, and DBPe data estimated from this method demonstrated very good correlation coefficients, r = 0.968 for SBP, r = 0.934 for MBP and r = 0.844 for DBP (see Fig. 2) with relation to neither gender nor to age. Also, MAD values between BPc and BPe data were acceptable within 5 mmHg. The good agreement between the two BP values strongly suggests that the BP calibration process conducted by each individual is very important; that is, each subject initially set their brachial BP data along with the PR and mNPV values (BPc0, PR0 and mNPV0) acquired from their own smartphone.
The availability of BP tracking was also found in all of the subjects except one (No. 11) without resetting this calibration procedure during the 1–2 weeks measurement period in the present study. In subject No. 11, who continued the study for a prolonged period of about 4 months, there was a considerable difference between BPc and BPe values of more than 30 mmHg; the reason for this is as yet unknown exactly, but perhaps is a displacement of the fingertip over the iPhone camera. This subject himself decided therefore to perform the calibration procedures twice instead of just once, as indicated by dashed lines in Fig. 3.
Overall, these results strongly suggest that this new cuffless technique, referred to as “rate resistance-index product”, based on the haemodynamic Ohm’s law, could allow smartphones, which are currently ubiquitous worldwide (Statista, 2016: Number of smartphone users worldwide from 2014 to 2020 (in billions)), to be employed as simple, stand-alone sphygmomanometers. Nevertheless, further research with larger in vivo and large-scale clinical experiments as well as technical improvements, as described below, would be required before this method could be fully accepted for routine clinical use.
As described in the Introduction, almost all cuffless BP estimation methods proposed previously have been based on the measurement of pulse wave velocity (PWV) or pulse transit time (PTT) with the use of various kinds of equations between cuff-based BP and PWV or PTT, on the basis of the Moens-Korteweg equation (Payne et al., 2006; Gesche et al., 2012; Mukkamala et al., 2015; Sharma et al., 2017; Ding et al., 2017; Nabeel, Jayaraj & Mohanasankar, 2017). A unique method combining PWV and PPG using machine learning to extract PPG features was recently reported (Kachuee et al., 2017). Also, smartphone-based BP estimation without cuff-based BP calibration using advanced machine learning algorithm was just recently reported (Luo et al., 2019). Apart from these two, all of these methods essentially require, sometimes frequently, a BP calibration that is based mainly on cuff-sphygmomanometry as a reference, and at present we cannot say for sure which of these methods is more convenient or reliable for routine use. One of the evaluation indices of these methods is measurement accuracy. The accuracies indicated by the r values in these previous methods were more or less 0.7 with a significant linear regression between cuff-based and estimated BP values, whilst in the present study the new method exhibited r values of 0.968, 0.934 and 0.844 respectively for the SBP, MBP and DBP data (Fig. 2). It should also be noted that the method described herein requires only a smartphone, so neither a PPG measuring unit nor a bio-amplifier for ECG detection are required. Taking these points into consideration, we believe that the present method is simple to use and has a reasonable accuracy as compared with the cuff-based sphygmomanometers with ESH standard used in this study: It is naturally noted that this method is available when the initial calibration is carried out using any type of commercial cuff-sphygmomanometer as a reference.
An important mathematical issue is that the assumption of constants k1 and k2 was used to derive the simplified relationships (Eqs. (5)–(7) expressed in the Methods section) based on the BP estimation in the present study, taking into account physiologically evidential findings from earlier literature (Obrist et al., 1978; Chau et al., 1978; Light, 1981; Sherwood, Dolan & Light, 1990; Sawada, Tanaka & Yamakoshi, 2001; Protogerou et al., 2007). Further research is, however, required to validate this issue through physiological experiments to make this method more secure and reliable. This validation aspect requires continuing investigation of the fundamental and mathematical background. However, our first essential step was planned simply to aim to compare the newly proposed method with cuff-based sphygmomanometry.
A further consideration, and possible disadvantage, with the use of the constants k1 and k2 in this new method, is that the assumed values of k1 and k2 do not always hold throughout measurements under resting conditions made over extended time periods. There is no choice at present but to avoid this issue by conducting a calibration procedure using the cuff-based BP measurements. It is therefore preferable to carry out, for example, weekly or monthly regular calibration procedures, although this is surely not ideal. However, this is not a major problem for people who wish to assess BP variation and regularly use a cuff-sphygmomanometer, since they can check BP values using only a smartphone when they like. The calibration procedures would be further simplified if the process of transferring the BP values to the smartphone was carried out automatically via wireless communication with a cuff-sphygmomanometer having a Bluetooth connection.
As has been shown above, good results were obtained by using Eqs. (6) and (7) to estimate SBP and DBP values respectively. These data were derived under the assumption that the haemodynamic Ohm’s law was valid. However, strictly speaking, this law actually applies to the mean value, i.e., MBP value. It is therefore necessary to investigate more appropriate estimation methods, based on the haemodynamic principles, for SBP and DBP values and this could then achieve even greater accuracy.
Careful contact and placement of the fingertip to cover the CMOS camera built into the smartphone is needed for stable determination of mNPV, and in fact also very important for obtaining an accurate BP estimation. Small differences in the contact state and the placement of the fingertip on the camera can produce a slight difference of the mNPV value, resulting in an erroneous BP estimation. It might be helpful for more practical use to design a jig embedded with a thin pressure sensor for gently fixing the fingertip and preventing relative movements as well as for monitoring the contact pressure between the fingertip and the CMOS camera. Further work is also suggested to search for a more suitable site such as the palm of a hand, to acquire a more stable PPG signal.
Although technical improvements such as those suggested above are needed for practical use, this new method offers a straightforward, sufficiently accurate (r > 0.84 and MAD < 5 mmHg) means of assessing SBPe, MBPe and DBPe with only a smartphone. At present it requires a calibration process using cuff-sphygmomanometry as a reference, however, a hybrid method in conjunction with, for example, our previous method (Matsumura et al., 2018) to remove such calibration procedure using PR0 and ARI0 could be worth considering, and is now under preparation to report elsewhere.
This new method, proposed as “rate resistance-index product”, based on haemodynamic principles, could potentially allow various types and models of smartphones and smart watches as well as finger-based pulse oximetry devices, to be used for BP estimation. It appears to have significant potential as a convenient substitute for traditional cuff-based sphygmomanometry.
Conclusions
The present study reported the successful development of a new cuffless blood pressure (BP) estimation method, experimental validation, and progress towards mobile healthcare. With this method we could estimate BP (BPe; systolic (SBPe), mean (MBPe) and diastolic BP (DBPe)), with much higher accuracy than achieved with earlier work, based on the so-called haemodynamic Ohm’s law, using pulse rate (PR) and a modified normalized pulse volume (mNPV; a measure of sympathetic arteriola constrictive activity in a finger), both also obtained from a smartphone-derived photoplethysmogram (PPG). Preliminary comparison experiments using 13 volunteers under resting conditions at home clearly demonstrated a good agreement between the cuff-based BP (BPc) and the BPe values through scatter plots and Bland-Altman error analyses as well as mean absolute differences between these two values. Fairly good tracking availability in terms of time series data of the BPc values against the corresponding BPe values was also confirmed in each subject during the study periods.
These results strongly suggest that this new cuffless technique, referred to as “rate resistance-index product”, based on haemodynamic principles, could allow smartphones, which are currently ubiquitous worldwide, to be employed as simple, stand-alone sphygmomanometers. However, further research with larger in vivo and large-scale clinical experiments as well as methodological and technical improvements, as described in Discussion, would be required before this method could be fully accepted for routine clinical use.
Nevertheless, the new method presented herein could potentially allow various types and models of smartphones and smart watches as well as finger-based devices, to be used for BP estimation. It appears to have significant potential as a simplified and convenient substitute for traditional cuff-based sphygmomanometry as well as for practical application to mobile healthcare.
Supplemental Information
The raw data of this study.
A total of 315 original data sets obtained from 13 volunteer subjects.