Evaluation of pulpal anesthesia and injection pain using IANB with pre-heated, buffered and conventional 2% lignocaine in teeth with symptomatic irreversible pulpitis—a randomized clinical study
- Published
- Accepted
- Received
- Academic Editor
- Luca Testarelli
- Subject Areas
- Anesthesiology and Pain Management, Clinical Trials, Dentistry, Drugs and Devices
- Keywords
- Buffered, Local anesthesia, Pre-warm, Irreversible pulpitis, Endodontics
- Copyright
- © 2022 Gandhi et al.
- Licence
- This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, reproduction and adaptation in any medium and for any purpose provided that it is properly attributed. For attribution, the original author(s), title, publication source (PeerJ) and either DOI or URL of the article must be cited.
- Cite this article
- 2022. Evaluation of pulpal anesthesia and injection pain using IANB with pre-heated, buffered and conventional 2% lignocaine in teeth with symptomatic irreversible pulpitis—a randomized clinical study. PeerJ 10:e14187 https://doi.org/10.7717/peerj.14187
Abstract
Background
The efficacy of 2% lignocaine is reduced in a hot tooth. Local aesthetic agents can be preheated and buffered to increase their effectiveness. The present investigation was carried out due to limited information concerning adult patients with symptomatic irreversible pulpitis in mandibular teeth.
Methods
A total of 252 individuals were included in the clinical trial in accordance with the selection criteria only after clinical study was registered with the Clinical Trial Registry of India (CTRI/2020/09/027796). Scores on the visual analog scale (VAS) and electric pulp test (EPT) on a 1–10 scale were recorded prior to the commencement of therapy. In this double-blinded study, patients were randomly divided by a co-investigator using computer randomisation (www.randomizer.org) into three groups, group A: inferior alveolar nerve blocks (IANB) with 2% lignocaine preheated at 42 °C (injected at 37 °C) (N = 84), group B: IANB of 2% lignocaine buffered with 0.18 ml of 8.4% sodium bicarbonate (N = 80) and group C: 2% lignocaine (N = 88). Excluding the dropouts of individuals (n = 11), wherein the anaesthesia failed, a total of 241 people were finally assessed 15 minutes after profound anaesthesia, endodontic access, and intraoperative pain were quantified using VAS. Pain on injection for all three groups was recorded immediately after IANB with VAS. The analysis was performed using one way ANOVA with Tukey’s post hoc test and Paired T-Test using SPSS version 21.
Results
Preheated, Buffered, and conventional 2% lignocaine showed statistically significant reduction in intraoperative pain (P < 0.001) compared to pre-operative but on inter-group comparison preheated and buffered showed highly significant pain reduction compared with conventional 2% lignocaine (P < 0.001).
Conclusions
Warm and buffered local anaesthetic (LA) were effective in reducing intraoperative discomfort than conventional LA. Preheated local anesthetics caused the least pain, followed by buffered local anesthetics, while conventional local anesthetics caused the most pain.
Introduction
In order to minimise discomfort during different dental, endodontic, and minor surgical treatments, local anaesthetic (LA) is necessary (Queiroz et al., 2015). In the majority of patients, it is challenging to achieve enough anaesthetic success for a “hot” tooth. According to the literature, inferior alveolar nerve blocks (IANB) using lignocaine in mandibular posterior teeth had a failure rate of 44%–81% (Claffey et al., 2004; Potočnik & Bajrović, 1999). There are a number of causes, including local tissue acidosis brought on by the production of lactic acid and its by-products, hyperalgesia offered on by inflamed pulp, and a lower resting membrane potential, but the most widely accepted theory is that tetrodotoxin-resistant sodium channels are to penalise (TTXr). Lignocaine makes it four times harder for these channels to close, and inflammation doubles the production of these molecules (Wells et al., 2007; Badrian et al., 2016).
Changes in injection method (Meechan, 1999), supplemental anaesthesia techniques (Yadav, 2015; Bhalla, Taneja & Chockattu, 2021), changes in anaesthetic liquid, etc. (Nagendrababu et al., 2019) are a few of the approaches utilised to increase the success rate of IANB in hot teeth. Lignocaine containing adrenaline usually have a pH range between 2.9–4.4 (Malamed, Tavana & Falkel, 2013). This pH is recommended to prolong the shelf life and to prevent oxidation of LA, but at the same time it shows reduction in its efficacy, burning sensation, slow anesthesia onset.
When used for mandibular or maxillary anaesthesia, elevating the pH of lignocaine by neutralising it with 8.4% sodium bicarbonate accelerates the dissociation rate and increases the concentration of uncharged base ions crossing the nerve membrane (Kattan et al., 2019).
Warming LA to 42 °C is another effective way to boost its effectiveness (Aravena et al., 2018; Tirupathi & Rajasekhar, 2020; Hogan et al., 2011). The LA molecule may infiltrate the nociceptor, causing sodium channels to block more promptly. This could be the result of local anaesthetics’ temperature-dependent, decreasing pKa (dissociation constant) value (Allen, Bunce & Presland, 2008). According to Powell (1987), lignocaine has a pKa of 7.57 at 40 °C and 7.92 at 25 °C. As a result, warming lignocaine may expedite the initiation of local anaesthetic and enhance its effectiveness.
The speed, location, and pH of the anaesthetic solution are only a few of the many aspects of local anaesthesia delivery that might induce pain. As a result, patients get anxious and postpone away necessary surgeries. A research by Gümüş & Aydinbelge (2019) demonstrated that pre-warming LA decreases injection discomfort. In a similar context, Palanivel et al. (2020) revealed that buffered LA caused the least discomfort during administration.
Since there is sporadic literature comparing the efficacy of preheated, buffered, and conventional LA on adult population, the present double-blinded randomized clinical study was designed aiming to evaluate the pulpal anesthesia and injection pain using IANB with pre-heated, buffered and conventional 2% lignocaine in teeth with symptomatic irreversible pulpitis. The null hypothesis was that there is no difference in efficacy of pulpal anesthesia and injection pain using IANB with pre-heated, buffered and conventional 2% lignocaine in teeth with symptomatic irreversible pulpitis.
Materials and Method
Study design, ethical approval, and clinical trial registry
This double-blind randomized clinical study was approved by the Sumandeep Vidyapeeth Institutional Ethics Committee (SVIEC/ON/DentBNPG18/D19047; date of approval 22/11/2019), India. The protocol was developed and registered at the clinical trial registry of India (CTRI/2020/09/027796). The current superiority trial was reported according to Consolidated Standards of Reporting Trials (CONSORT) guidelines (Schulz, Altman & Moher, 2010). Written informed consent was obtained from all participants in this study.
Sample size
In a one-way ANOVA study, sample sizes of minimum 60, 60 and 60 were obtained from the three groups whose means were compared. The total sample of 180 subjects achieves 80% power to detect differences among the means versus the alternative of equal means using an F test with a 0.05 significance level. The size of the variation in the means is represented by their standard deviation which is 30.0 the common standard deviation within a group is assumed to be 1.13. Between groups, the one way analysis of variance with multiple comparison tested at 5% level. The sample size formula used was: (Zalpha +Zbeta)2*Sqrt(n*delta2/2kS2), where Zalpha = 1.96; Zbeta = 0.84; n = total number of groups = 3; delta = mean difference = 30.0; k = degrees of freedom = n-1 = 2; S = standard deviation = 1.13.
However number of patients enrolled in the study were 252 divided into in following three groups: (A) preheated 2% lignocaine, (n = 84); (B) buffered local anesthesia, (n = 80); and (C) conventional 2% lignocaine, (n = 88).
Selection criteria
Patients were selected as per the inclusion: patients among 18 to 60 years of age with mandibular hot teeth (Symptomatic irreversible pulpitis), having actively experienced moderate to severe pain on a visual analog scale (VAS) scale of five or more were included in the study. Exclusion criteria: Patients with known hypersensitivity to Lignocaine and sodium bicarbonates, who had undergone cardiac surgery in the last six months, pregnant or lactating females, or with necrosed teeth with sinus or swelling, severe periodontitis and poor oral hygiene, cracks, fracture, and open apex were excluded from the study.
Randomization and allocation concealment
A postgraduate student assessed the eligibility of five hundred and twenty-one patients based on clinical examinations, radiographs, and pulp sensibility tests. Clinically tooth having spontaneous/lingering pain/nocturnal pain with moderate to deep carious lesion and absences of tenderness on percussion and delayed response to the electric pulp test (EPT) were taken for further radiographic examination. Tooth with radiolucency involving enamel, dentin, and approaching pulp was selected. All the radiographs were taken with a long cone and paralleling technique using a positioning indicator device. Two hundred and fifty-two patients meet the selection criteria and agreed to participate in the trial. Co-investigator implemented the random sequence generation and allocation concealment. Randomization was done by computer randomization (https://www.randomizer.org/) and patients were assigned into three groups.
The allocation concealment ratio was 1:1:1. This was done by inserting the LA cartridges in sequentially numbered sealed opaque envelopes. The envelopes were marked with the randomization code. As soon as the patient was placed in the intervention group, the number was noted in the patient’s case sheet and decoded at the end of the trial.
Blinding
The entire procedure was double-blinded to avoid bias. The primary investigator and the patient both were blinded to the groups allotted. The operator directly received an aspirating metal syringe loaded with the cartridge of lignocaine; pre-heated lignocaine or buffered lignocaine with a 27-gauge needle attached to the tip of the unit.
Clinical procedure
Patients were sensitized to a (1 to 10-point) VAS scale. This scale was given to the patient to choose thrice: the first time was before the injection, second time after receiving the injection, and the third after entering the pulp chamber and a pre-operative VAS score was recorded. Pre-operative pulp sensibility test was recorded using the electric pulp test (EPT). The patient was explained about the test and the tooth was checked first followed by the affected tooth. Patients were asked to indicate when a tingling sensation occurs to him/her, and the response of the affected tooth was noted down in numbers.
For group A—The preparation of preheated local anesthesia was done according to method described by Allen, Bunce & Presland (2008) and Davidson & Boom (1992). A 1.8 ml cartridge of commercially accessible 2% lignocaine hydrochloride with 1:80,000 adrenaline (Lignospan special, Septodont Healthcare India) was placed in a composite warmer (12 VDC, 2000Mpa, 24W0 power supply; AR Heat), for 4 min. Two cartridges were placed in the heating slot of the warmer and the thermostat is set in such a way that a temperature of 42 °C was obtained for the anesthetic liquid. The rubber cap of the second cartridge was removed and a thermometer was used to check the temperature of the anesthetic solution, as it is ascertained at 37 °C (body temp), the first 1.8 ml cartridge was administered to the patient.
For group B—The preparation of buffered local anesthesia was done according to a previous study (Saatchi et al., 2015). The buffered local anesthetic solution has a shelf-life of one week, but it was prepared fresh once every two days for maximum efficacy. Under sterile conditions, 0.18 ml from a 1.8-ml cartridge of 2% Lignocaine with 1:80,000 adrenaline was drawn and replaced with 0.18 ml 8.4% sodium bicarbonate using a 1 ml plastic syringe and stored in the refrigerator. The cartridge was inverted five times to mix the solution. As a result, no precipitation was formed. It was shaken until the solution was clear; this ensured that the sodium bicarbonate was completely dissolved. The cartridge was then loaded into a metal syringe and injected.
For group C—Preparation of conventional group – Conventional nerve block with 1.8ml of 2% lignocaine with 1:80,000 adrenaline was injected. IANB in all the three experimental groups was given with a metal syringe with 27-G, a 1.5-inch needle attached to a standard aspirating dental injection syringe about 1 mm, and 1.8 ml of the solution was deposited slowly (2 min). Immediately after injection, VAS was used to evaluate the injection pain for all the experimental groups.
All the patients were asked to wait for 15 min for the profound anesthesia to be achieved. Subjective symptoms like tingling sensation, numbness of lower lip, buccal and lingual periosteum on the respective side of jaw were considered, whereas objective symptoms like EPT (Parkell Gentel Pulse vitality tester) of concerned tooth was done, negative response to EPT was considered as effective anesthesia. Those patients who do not showed subjective and objective symptoms were given supplementary intra-ligamentary injections and were excluded from the study (consort flow chart).
Isolation was performed with the help of a rubber dam fifteen minutes after the injection. Excavation of caries was done along the walls of the tooth and lastly, the pulpal roof was prepared. Access cavity preparation was done with help of endo access bur to design the access cavity. After entering the pulp chamber and intra-operative VAS score was recorded as intra-operative reading. Further, the endodontic treatment was performed as per the standard methods and protocol by the primary investigator.
Statistical methods
The obtained data were tabulated and statistically analyzed using SPSS version 21 and p-value and Chi-square Value, one way ANOVA with Tukey’s post hoc test, and paired t-test were applied. For the statistical test between the group, a one-way analysis of variance with multiple comparison tests at the level of significance was set as 5%.
Results
Demographic data
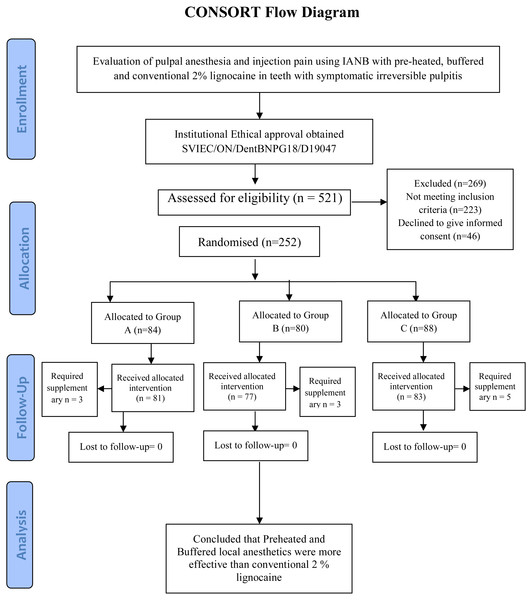
The patients enrolled in the clinical trial are presented on the CONSORT 2010 flow diagram (Fig. 1). Total of 252 patients were included in present study of which 11 patients were dropped out as lip numbness was not achieved after 15 min of INAB and considered as failure due to the wrong technique. So, 241 patients were included for final evaluation. Out of the total enrolled patients, 119 were male, while 122 were female. The age of 41 patients was between (18–25) years of age, 82 patients were between (26–36) years, 66 patients were between (37–46) years of age and the remaining 52 patients were between (47–60) years of age.
Figure 1: CONSORT 2010 flow diagram.
Pre-Intra operative VAS score
The mean pre-operative pain using a 10-mm Visual Analog Scale (VAS) was 7.28 mm ± 1.26 mm, for Group A. For Group B mean VAS score was 6.88 mm ± 1.23 mm, and for Group C score was 6.88 mm ± 1.24 mm (Table 1). On comparing the means of all three groups no statistical difference was found in the pre-operative pain values. While the mean of Intra-operative pain for Group A was 1.59 mm ± 1.03 mm, for Group B 1.69 mm ± 1.07 mm, and Group C was 3.54 mm ± 2.34 mm. This shows that all three local anesthetic agents were highly effective in reducing pain (P value <0.001).
| Groups | N = 241 | Mean | Std. deviation | Mean difference | t-value | p-value | |
|---|---|---|---|---|---|---|---|
| Group A | VAS Pre | 81 | 7.28 | 1.26 | 5.69 | 36.075 | <0.001 |
| VAS Post | 81 | 1.59 | 1.03 | ||||
| Group B | VAS Pre | 77 | 6.88 | 1.23 | 5.18 | 38.120 | <0.001 |
| VAS Post | 77 | 1.69 | 1.07 | ||||
| Group C | VAS Pre | 83 | 6.88 | 1.24 | 3.34 | 12.331 | <0.001 |
| VAS Post | 83 | 3.54 | 2.34 |
Table 2 shows an inter-group comparison between all the three experimental groups for the reduction in intra-operative pain, there was no statistically significant difference (P = 0.183) between Group A (Preheated LA) and Group B (Buffered LA). Whereas there was a highly significant difference (P < 0.001) between Group A (Preheated LA)—Group C (Conventional LA) and between Group B (buffered LA)—Group C (Conventional LA). This indicates that buffered and preheated local anesthetic solutions are more efficient in reducing pain in patients with symptomatic irreversible pulpitis in comparison to conventional 2% local anesthetic agents.
| Dependent variable | Group | Mean difference | Std. Error | p-value | |
|---|---|---|---|---|---|
| VAS Difference (pre-intra) | Group-A | Group-B | 0.51 | 0.28 | 0.183 |
| Group-C | 2.35 | 0.28 | <0.001* | ||
| Group-B | Group-C | 1.84 | 0.28 | <0.001** | |
Notes:
The values marked with (* and **) exhibited significant difference.
Pain on injection
The mean pain on LA administration using VAS (Visual Analog Scale) for Group A was 1.35 mm ± 1.09 mm, Group B was 2.08 mm ± 1.27 mm, and Group C was 3.19 mm ± 0.93 mm. Table 3 shows the mean difference between Group A and Group B was −0.73 mm ± 0.17 mm and between Group A and Group C was −1.84 mm ± 0.17 mm stating that there statistically significant difference between the groups (P value <0.001). Correspondingly comparing Group B with Group C showed a mean difference of −1.11 mm ± 0.17 mm and a p-value of <0.001 thus indicating there was a statistically significant difference between them concerning pain on injection. This shows that preheated LA showed the least pain on injection followed by buffered and conventional LA.
| Dependent variable | Group | Mean difference | Std. Error | p-value | |
|---|---|---|---|---|---|
| Pain on injection | Group-A | Group-B | −0.73 | 0.17 | <0.001 |
| Group-C | −1.84 | 0.17 | <0.001 | ||
| Group-B | Group-C | −1.11 | 0.17 | <0.001 | |
Notes:
P values 0.05 are corellated with significant difference.
Discussion
In the current clinical exploration, patients with symptomatic irreversible pulpitis were evaluated to determine the effectiveness of inferior alveolar nerve block in relieving pain using pre-heated, buffered, and standard 2% lignocaine. The study’s null hypothesis was rejected in light of the findings.
Clinical dentistry has changed from being an unpleasant and traumatic experience to one that is substantially less uncomfortable and more satisfying because to the efficacious use of LA. Profound anaesthesia during root canal therapy not only helps the patient but also frees the dentist from worrying about unanticipated movements or reactions from the patient. Patients with symptomatic irreversible pulpitis (hot tooth) and challenges with mandibular teeth sometimes have trouble achieving enough anaesthetic effect (Sahu, Kabra & Choudhary, 2019). Therefore, amendments are suggested to increase efficacy.
Changing the pH and temperature of the anaesthetic solution is the most productive technique to improve efficacy and lessen pain during injection, according to a clinical trial on minors (Kurien, Goswami & Singh, 2018). Warming the local anaesthetic solution to body temperature (37 °C) before administration seemed to lessen pain during intraoral local anaesthesia administration (Aravena et al., 2018; Tirupathi & Rajasekhar, 2020) and buffered local anaesthetic (Kattan et al., 2019) solutions in adult patients, according to a number of randomised clinical studies and systematic reviews on prewarmed and unwarmed LA solution. However, there is scant information comparing preheated, buf. So the current study was created.
The Visual Analog Score was used to assess the decrease in intra-operative pain and pre-operative discomfort. Because the VAS is dependable, repeatable, and simpler for patients to comprehend and record, we chose to utilise it (Hawker et al., 2011).
The effectiveness of IANB is often assessed by the subjective and objective symptoms that patients experience after being under anaesthesia, however an electric pulp tester (EPT) is a more accurate way to assess pulpal anaesthesia (Warren et al., 2017). Progressive pulpal anaesthesia is defined as no response to EPT. Contrasted with the study by Certosimo & Archer (1996), which demonstrated that a “no reaction” at an 80-reading guaranteed pulpal anaesthesia in crucial asymptomatic teeth For a longer shelf life, anaesthetic solutions sold commercially are acidic (Malamed, Tavana & Falkel, 2013). Unfortunately, the LA solution’s acidity has several drawbacks that affect how well it works in clinical settings, so we need to modify it. Buffering local anaesthesia is one such improvement. It is made by mixing 1.8 ml of LA with 0.18 ml of sodium bicarbonate, 8.4%, which results in the creation of carbon dioxide and water (Afsal et al., 2019). Since carbon dioxide directly depresses the axon, concentrates LA into the nerve trunk (ion trapping), and changes LA into an active cationic state, it helps buffered LA work more effectively.
In patients with a hot tooth, buffering LA enhances the chance of effective anaesthesia by 2.29 times, according to a systematic review by Kattan et al. (2019). Kurien, Goswami & Singh (2018) and Saatchi et al. (2018) both endorse the same. However, Schellenberg et al. (2015) and Hobeich et al. (2013) reported dissenting findings. Different populations involved, non-standard buffering approaches, varying injection methodologies, and various assessment techniques can all lead to variances (Palanivel et al., 2020).
Pre-heating local anaesthetic at 42 °C is another method for increasing LA effectiveness in inflamed pulp (Afsal et al., 2019). By blocking sodium channels, conventional LA prevents a change in the nerve impulse’s course of propagation. By increasing membrane fluidity, which makes it easier for lignocaine to pass and reach the effective concentration faster, and by densely expressing TRPV1 channels in trigeminal tissue, warming at 42 °C aids in faster blockage of the sodium channels (Afsal et al., 2019). According to Alonso, Perula & Rioja (1993), there was a negative correlation between temperature and pain, with 10 °C having the greatest mean pain level and the following temperatures: 18 °C, 37 °C, and 42 °C. In order to prevent any negative reactions from happening to the oral tissue, pre-heated LA was administered at 37 °C, or at the physiological tissue pH. According to Davidson & Boom (1992), subcutaneous infusion of LA at body temperature (37 °C) lowers pain severity after minor oral surgery.
In this investigation, the warmed group’s intra-operative agony was much lower than it was in the traditional LA group. There were no significant differences between pre-warmed and traditional LA, which was in contrast to Ram, Hermida & Peretz (2002) but in conformity with Tirupathi & Rajasekhar (2020) and Aravena et al. (2018). The modified Behavioral Pain Scale (BPS), which is difficult to comprehend, was employed as the evaluation criterion, which may have contributed to the disparity between the research populations. The secondary result of pain during injection was investigated, and preheated and buffered 2% lignocaine was shown to cause the least discomfort. This finding was consistent with a clinical investigation by Gümüş & Aydinbelge (2019).
The study’s shortcoming is that just one concentration of sodium bicarbonate (8.4%) was utilised to buffer LA; more research carried out using different concentrations is warranted. The same research design must be used to analyse patients with systemic disorders (such as hypertension, diabetes mellitus, and other systemic illnesses).
Conclusions
Considering the limitations of the study, we would like to conclude that preheated, buffered, and conventional local anesthesia was effective in reducing pain in symptomatic irreversible pulpitis. When compared to standard LA, the warmed and buffered LA was more successful in reducing intraoperative discomfort. Preheated local anaesthetics and buffered local anaesthetics caused the least amount of discomfort during administration, but the standard group caused higher pain. Future RCTs with a larger sample size will be beneficial to confirm the findings.